Appendix E : Health and medical Care Technical Requirements

EPIDEMIOLOGICAL EVIDENCE-BASED PROBABILISTICRISK ASSESSMENT (PRA)
E.1 PURPOSE
Perseverance, nicknamed Percy, is a car-sized Mars rover designed to explore the crater Jezero on Mars as part of NASA’s Mars 2020 mission. It was manufactured by the Jet Propulsion Laboratory and launched on 30 July 2020, at 11:50 UTC. Confirmation that the rover successfully landed on Mars was received on 18 February 2021, at 20:55 UTC. As of 31 August 2021, Perseverance has been active on Mars for 189 sols (194 Earth days) since its landing. Following the rover’s arrival, NASA named the landing site Octavia E. Butler Landing.
E.2 EPIDEMIOLOGICAL EVIDENCE-BASED PROBABILISTICRISK ASSESSMENT (PRA)
E.2.1 Background
The Health and Medical Care Technical Requirements reference an epidemiological evidence based PRA as a decision support tool to aid clinical stakeholders, engineering teams, and medical mission planners in the development of medical capabilities to treat the most likely medical conditions that may occur for a specific mission. The purpose of this Appendix is to provide background on this PRA and provide an outline of steps to consider during the process.
Epidemiological evidence-based medical PRA is a comprehensive, structured, and logical analysis method aimed at providing probability of occurrence of medical conditions based on past spaceflight experience coupled with terrestrial occurrences of medical conditions. Presently, The Integrated Medical Model (IMM) that was developed by the Human Research Program is a stochastic decision support tool that is available for use by clinical stakeholders, spaceflight mission planners, and medical system designers in assessing risks and optimizing medical systems. Other approved PRA decision support tools may also be utilized to meet the intent of the health and medical care technical requirements. Refer to section 3 for Health and Medical Technical Requirements description.
E.2.2 Integrated Medical Model (IMM) Overview
The IMM incorporates “best evidence” with data from past missions, computer models, and comparable populations on Earth, to provide a quantifiable assessment of medical risk for a given mission scenario. The IMM also identifies medical resources, such as equipment and supplies, which are necessary for treating the medical conditions most likely to occur during the mission. Using the Monte Carlo simulation technique (a random sampling of the data inputs as described by their statistical distribution), the IMM can forecast medical outcomes, helping to provide more appropriate medical support for flight crews. The medical conditions addressed by the IMM range from minor conditions (such as headaches and nasal congestion) to more serious conditions (such as sudden cardiac arrest and kidney failure).
The IMM currently derives estimates of fire/smoke/toxic inhalation risks from the ISS PRA fire model. IMM uses incidence data generated by independent predictive health models and by Bayesian analysis. The incidence of these events can be used as estimates for other vehicles, if appropriate, or updated data can be provided for the specific vehicle.
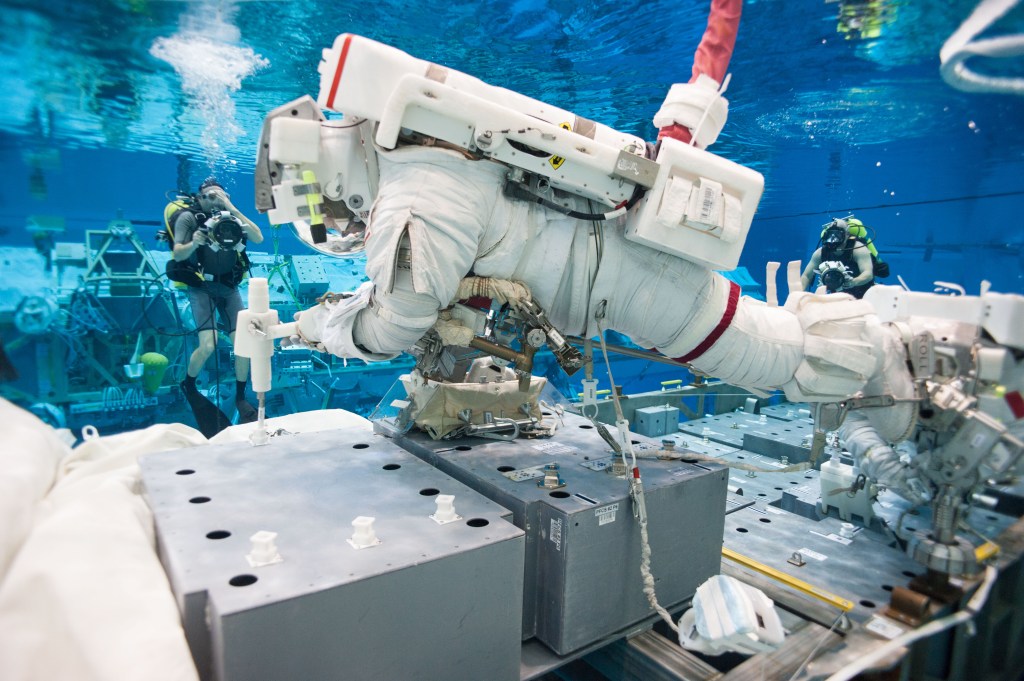
The IMM requires the user to provide the mission duration, location, number of EVAs and crew attributes (for example quantity or sex) and will generate the type and probability of occurrence (likelihood) of medical events. IMM also assumes that the crew selection and Health Stabilization Program technical requirements are followed to ensure that the crew is in the best health posture prior to the mission. Refer to Table E.2-1—Sample IMM Output.
Table E.2-1—Sample IMM Output
| Medical Condition | Likelihood | |
|---|---|---|
| 1 | Late Insomnia | 13.85 per mission |
| 2 | Skin Abrasion | 9.86 per mission |
| 3 | Skin Rash | 9.83 per mission |
| 4 | Eye Abrasion | 7.42 per mission |
| 5 | Late Headache | 5.25 per mission |
| 6 | Space Motion Sickness (SAS) |
4.37 per mission |
| 7 | Diarrhea | 3.53 per mission |
| 8 | Nasal Congestion | 3.51 per mission |
| 9 | Respiratory Infection | 3.46 per mission |
| 10 | Back Injury | 3.41 per mission |
| 11 | Barotrauma (Ear/Sinus Block) |
3.28 per mission |
| 12 | Back Pain (SAS) | 3.15 per mission |
| 13 | Insomnia (SAS) | 2.70 per mission |
| 14 | Shoulder Sprain/Strain | 2.43 per mission |
| 15 | CO2 Headache | 2.15 per mission |
| 16 | Headache (SAS) | 2.11 per mission |
| 17 | Spaceflight Associated Neuro-ocular Syndrome (SANS) |
2.08 per mission |
| 18 | Urinary Tract Infection | 1.44 per mission |
| 19 | Skin Infection | 1.38 per mission |
| 20 | Elbow Sprain/Strain | 1.32 per mission |
| 21 | Ankle Sprain/Strain | 1.22 per mission |
| 22 | Allergic Reaction | 1.18 per mission |
| 23 | Pharyngitis | 1.17 per mission |
| 24 | Constipation | 1.02 per mission |
| 25 | Neck Injury | 0.99 per mission |
| 26 | Mouth Ulcer | 0.96 per mission |
| 27 | Dental Caries | 0.88 per mission |
| 28 | Knee Sprain/Strain | 0.78 per mission |
| 29 | Paresthesia [Extravehicular Activity (EVA)] |
0.65 per mission |
| 30 | Indigestion | 0.64 per mission |
| 31 | Eye Chemical Burn | 0.64 per mission |
| 32 | Sinusitis | 0.64 per mission |
| 33 | Hearing Loss | 0.57 per mission |
| 34 | Wrist Sprain/Strain | 0.55 per mission |
| 35 | Eye Infection | 0.53 per mission |
| 36 | Hip Sprain/Strain | 0.45 per mission |
| 38 | Fingernail Delamination [Extravehicular Activity (EVA)] |
0.40 per mission |
| 39 | Otitis Externa | 0.32 per mission |
| 40 | Otitis Media | 0.30 per mission |
| 41 | Hemorrhoids | 0.22 per mission |
| 42 | Lower Extremity Stress Fracture |
0.13 per mission |
| 43 | Urinary Retention | 0.11 per mission |
| 44 | Skin Laceration | 0.11 per mission |
| 45 | Influenza | 0.11 per mission |
| 46 | Finger Dislocation | 0.11 per mission |
| 47 | Shingles | 0.11 per mission |
| 48 | Dental Abscess | 0.068 per mission |
| Table E.2-2—Medical Conditions Considered of High Likelihood or High Consequence for Spaceflight Missions summarizes the most common conditions that need to be assessed for missions up to 6 months. The items in bold and with an asterisk are the most common and should be considered for any mission duration. |
Table E.2-2—Medical Conditions Considered of High Likelihood or High Consequence for Spaceflight Missions
| Category | Specific Condition |
|---|---|
| Environmental or spaceflight induced medical conditions | Acute radiation syndrome Allergic reaction * Altitude sickness Anaphylaxis * Back pain (space-adaptation related) * Barotrauma (ear/sinus block) Burn (thermal) Burns secondary to fire Celestial dust exposure Choking/obstructed airway Cold injury (chilblains frostbite) Constipation (space-adaptation related) * Decompression sickness Embolism Electrical injury Epistaxis (nosebleed, space adaptation related) EVA-related dehydration Headache (CO2 related) * Headache (space-adaptation related) * Hearing loss (noise related) Heat illness Hypothermia Medication adverse reaction Nasal congestion (space-adaptation related) * Nutritional deficiency Space motion sickness (space-adaptation related) * Smoke/combustion product inhalation Toxic inhalation injury Urinary incontinence (space-adaptation related) * Urinary retention (space-adaptation related) * |
| Ophthalmic conditions | Acute glaucoma Chemical eye injury * Corneal abrasion * Corneal ulcer Eye foreign body * Eye infection Eyelid/anterior eye infection Loss of vision Penetrating eye injury Retinal detachment/injury SANS |
| Ear, nose, and throat conditions | Acute sinusitis Cerumen impaction Epistaxis (nosebleed) Hearing loss Otitis externa Otitis media Pharyngitis Respiratory infection |
| Dental/oral conditions | Caries Crown loss Dental abscess Filling loss Fractured tooth/Exposed pulp Oral ulcer Tooth loss (avulsion/luxation) |
| Cardiovascular conditions | Acute coronary syndrome Angina/Myocardial infarction Cardiac dysrhythmias (atrial fibrillation/flutter) Cardiogenic shock Gravity transition orthostatic intolerance * Hypertension Sudden cardiac arrest Traumatic hypovolemic shock Venous thromboembolism |
| Pulmonary and other chest conditions | Chest injury – Blunt Chest injury – Penetrating Reactive airway/asthma Respiratory tract infection (lower) Respiratory tract infection (upper) |
| Gastrointestinal and other abdominal conditions | Abdominal injury – Blunt Abdominal injury – Penetrating Abdominal wall hernia Acute cholecystitis / Biliary colic Acute diverticulitis Acute pancreatitis Appendicitis Constipation * Diarrhea * Gastroenteritis Hemorrhoids Indigestion * Reflux/esophagitis Small bowel obstruction |
| Genitourinary conditions | Abnormal uterine bleeding Acute kidney injury Acute prostatitis Bacterial vaginosis Nephrolithiasis Urinary tract infection * Unprotected intercourse Vaginal yeast infection * |
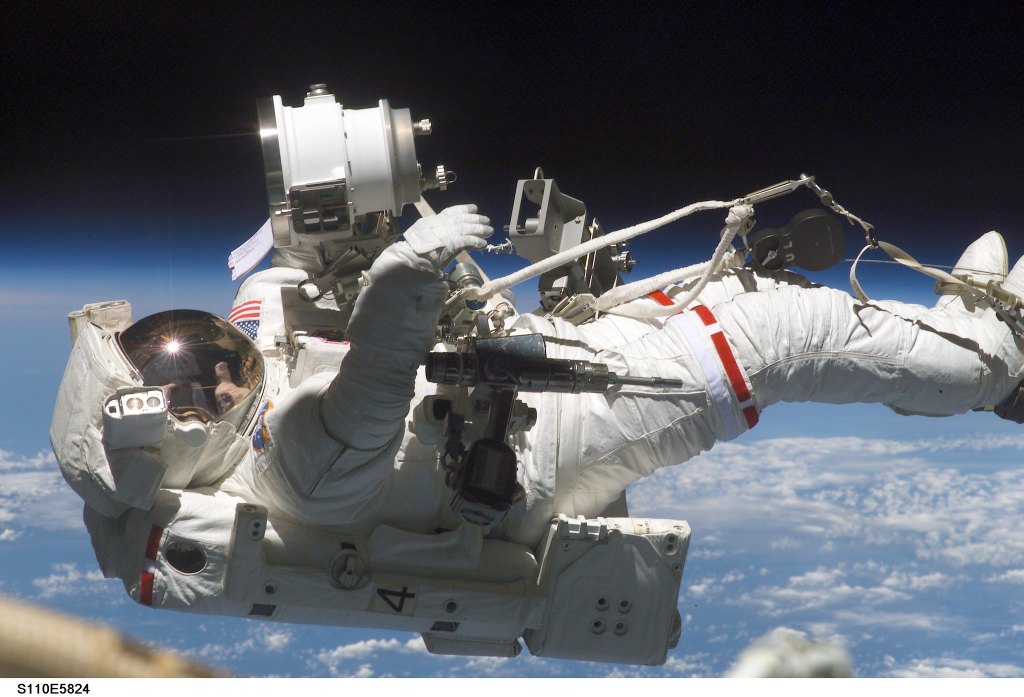
| Musculoskeletal conditions | Acute arthritis Acute compartment syndrome Back injury (sprain/strain) Dislocation (finger, elbow, shoulder) Fingernail delamination (EVA related) Fracture (finger, hand, wrist/arm, distal leg, hip/proximal femur, thoracolumbar spine, cervical spine) Hand injury (EVA related) Joint sprain/strain (shoulder, elbow, wrist, hip, knee, ankle) Lower extremity stress fracture Muscular sprain/strain Neck injury (sprain/strain) Overuse injury – Upper or lower extremity Paresthesia Subungual hematoma Suit contact injury (EVA related) Vertebral disc injury |
| Dermatological conditions | Burn – Chemical, skin Cellulitis – Bacterial skin infection * Herpes zoster (Shingles) Skin abrasion * Skin laceration * Skin rash * Toxic dermal exposure Viral/fungal skin infection |
| Neurologic conditions | Benzodiazepine/Opiate overdose Cerebrovascular accident Gravity transition neurovestibular disturbance * Headache * Head trauma (major) Head trauma (minor) Neurogenic shock Neuropathy (Central – impingement) Paresthesia Seizure |
| Psychological, cognitive, or behavioral conditions | Acute stress * Adjustment reaction * Anxiety/panic * Apathy/low motivation Cognitive disturbance * Delirium Depression Grief reaction Insomnia/sleep disturbances/circadian misalignment * Interpersonal conflict (i.e., team, ground, family) * Lack of meaningful work and/or monotony Mood disturbance (e.g., irritability) * Neurocognitive disorders (adjustment, mood, anxiety, trauma-related, or stress-related) Psychosis Relationship problems (family, crew, mission support personnel) Work overload/burnout/exhaustion |
| Other conditions not captured elsewhere | Anemia/Iron deficiency Sepsis |
| Conditions noted with an asterisk (*) should be addressed on every mission regardless of the DRM parameters. |
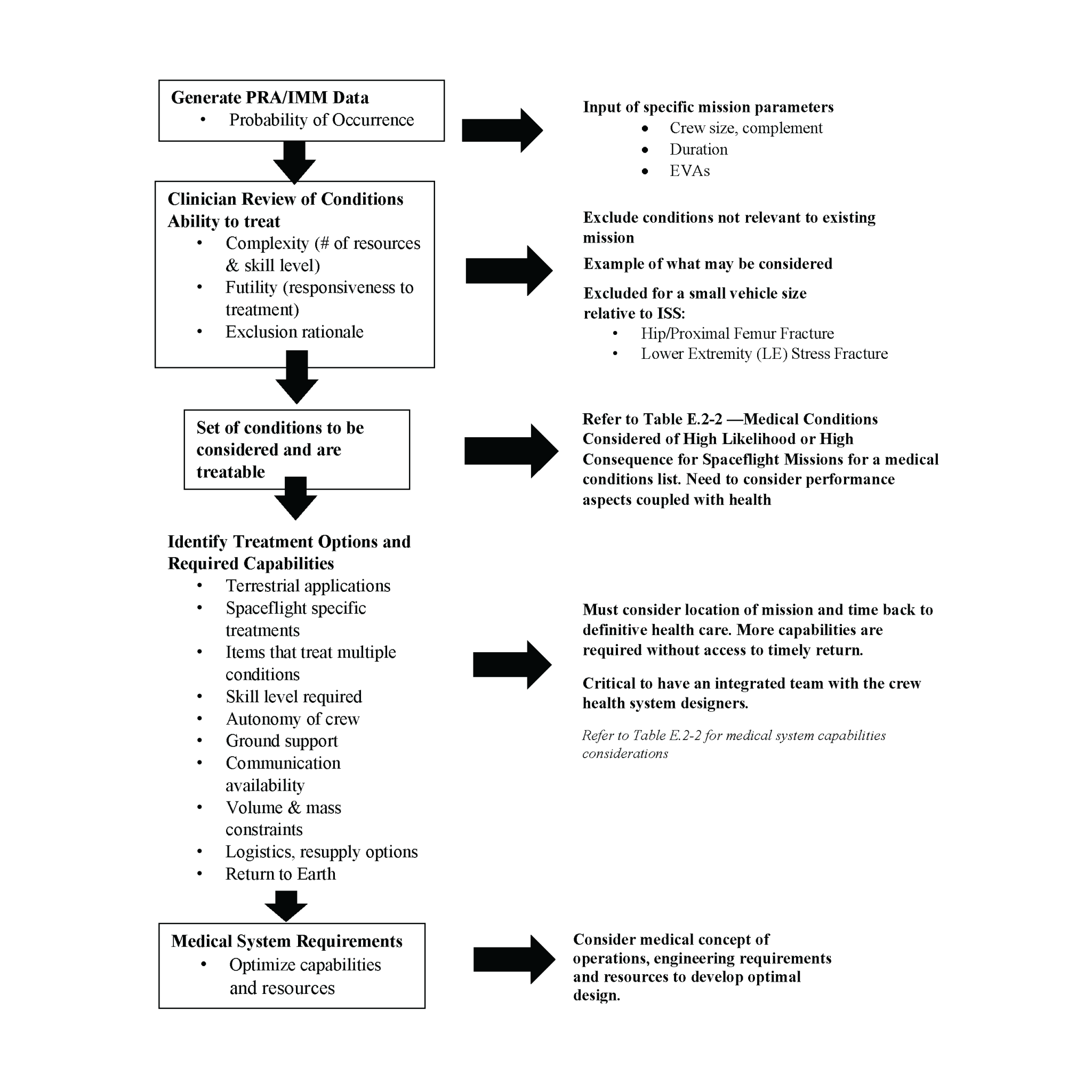
E.2.3 Medical System Development using PRA Integrated Medical Model (IMM) Data
The IMM output of probability of occurrence of medical conditions that may occur in-mission is a quantitative starting point for stakeholders to consider while developing an in-mission medical system. One limitation is that IMM was developed for application to ISS missions, but it may be applied to other design reference missions if the appropriate limitations are considered during interpretation of results. Figure E.2-1—Outline for the Use of PRA Data to Aid in the Generation of a Medical Conditions List, outlines the steps to utilize the PRA/IMM data in the development of a health and medical care system.