3.0 Health and Medical Care

Contents
- 3 HEALTH AND MEDICAL CARE
- 3.1 Medical Management
- 3.2 Selection and Recertifications
- 3.3 Pre-mission Preventive Health Care
- 3.4 In-Mission Preventive Health Care
- 3.5 In-Mission Medical Care
- 3.6 Medical Evacuation
- 3.7 In-Mission Evacuation to definitive Medical Care Facilities
- 3.8 Palliative Comfort care
- 3.9 Termination of Care
- 3.10 Crewmember Mortality
- 3.11 Terrestrial Launch/Landing Medical Support
- 3.12 Terrestrial Launch/Landing - Definitive Medical Care Facility (DMCF)
- 3.13 Certification of Training Plans for Launch/Landing Medical Team
- 3.14 Post-Mission Health Care
- 3.15 Post-Mission Reconditioning
- 3.16 Post-Mission Long-Term Monitoring
3 HEALTH AND MEDICAL CARE
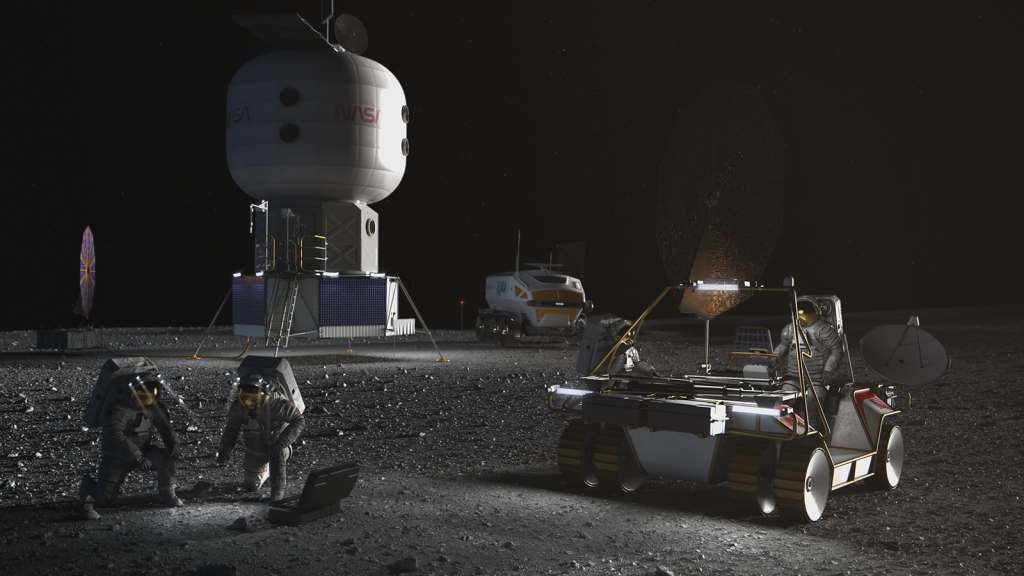
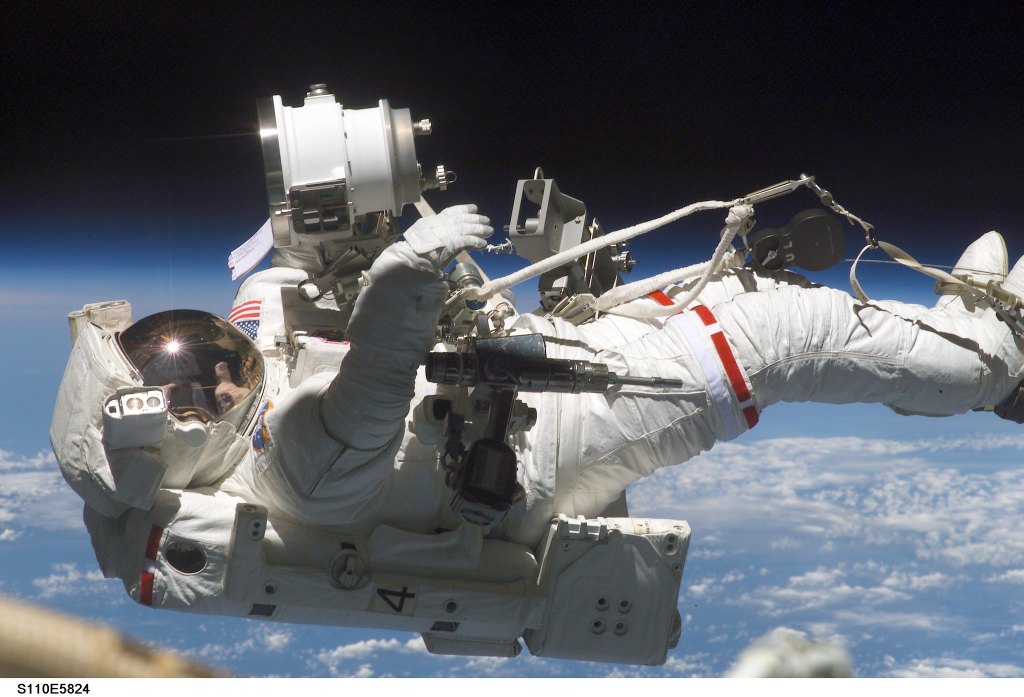
Crewmember health care starts at selection, is implemented throughout training, spaceflight missi Artemis Food Risk – Loss of Food/Nutrition and Food Poisoning ons, and post-mission reconditioning, and continues past retirement from the astronaut corps via the TREAT (To Research, Evaluate, Assess, and Treat) Astronauts Act, which authorizes NASA to monitor, diagnose, and treat medical and psychological conditions associated with spaceflight for NASA (US government) astronauts. Deeply rooted in preventive medicine, aerospace medicine puts an emphasis on preventive care, while being prepared to respond to the known physiological and psychosocial challenges of spaceflight, as well as unexpected illness and injury that could afflict crewmembers due to their active lifestyles, their training for flight, their missions in space, and their post-mission recovery.
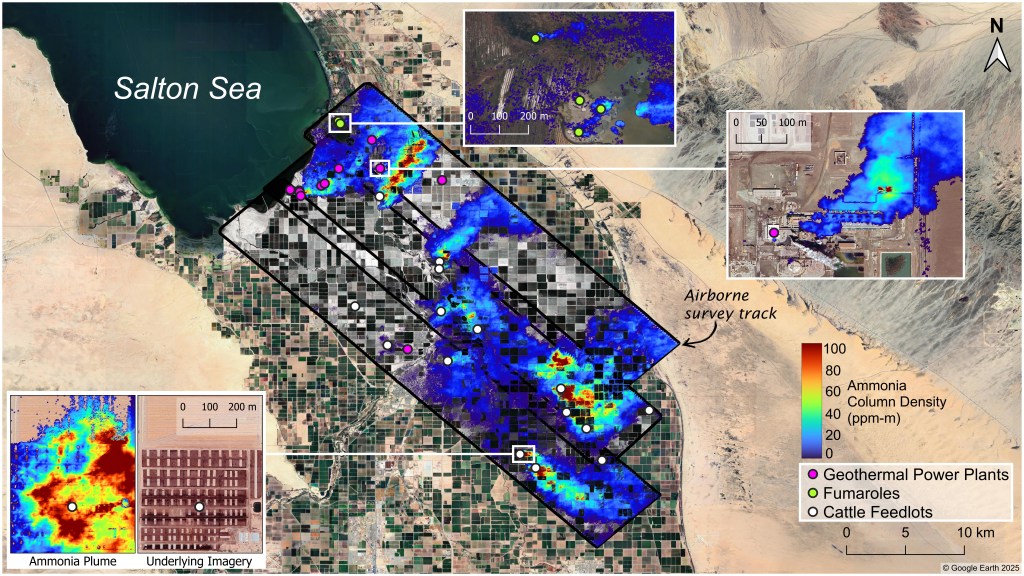
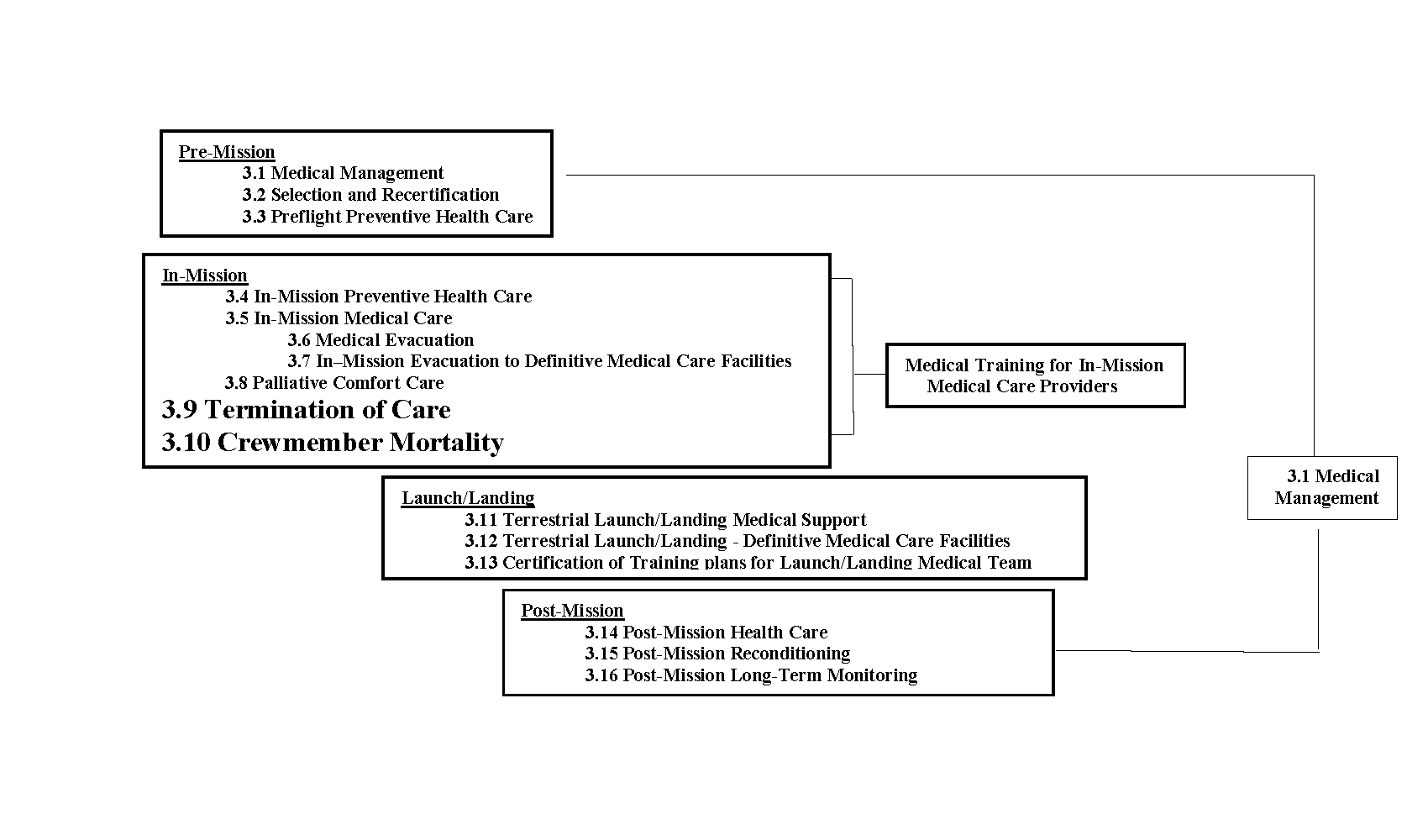
The following technical requirements reflect this comprehensive approach to crewmember health and well-being, addressing screening, preventive health strategies, medical care, contingencies during launch and landing, and post-mission healthcare, reconditioning and long-term monitoring. Refer to Figure 3.1-1—Health and Medical Care Technical Requirements Overview for an overview of the Health and Medical Care technical requirements.
Of note, the term “in-mission” which is introduced in this section of this NASA Technical Standard covers all phases of the mission, from launch, through landing on a planetary body and all surface activities entailed, up to landing back on Earth. Appendix D contains a requirements compliance matrix which provides additional information relative to health and medical care technical requirements described in this section
Figure 3.1-1—Health and Medical Care Technical Requirements Overview
3.1 Medical Management
[V1 3000] All terrestrial and in-mission medical aspects included in this NASA Technical Standard shall be in accordance with current U.S. and appropriate partners medical care standards, with limitations as imposed by mission constraints, and managed by the Flight Medicine team, which includes, but is not limited to: the Flight Medicine Clinic, Flight Surgeon, Deputy Flight Surgeon, and their designees, including the in-mission medical care providers (Crew Medical Officers).
3.2 Selection and Recertifications
[V1 3001] Crewmembers shall be medically and psychologically selected and annually recertified following the guidance in OCHMO-STD-100.1A, NASA Astronaut Medical Standards Selection and Annual Recertification.
[Rationale: Medical and psychological screening is required for all crewmembers that fly on/to NASA vehicles or otherwise interact with NASA crewmembers. Medical screening reduces crewmember health risks in-mission and post-mission, along with increasing mission success. The scope of initial screening may be influenced by mission duration, distance from Earth, and criticality of individual crewmember functions (pilot, extravehicular activities (EVAs), robotic operations, spaceflight participant, etc.). Similarly, mission-specific screening, if required, will consider mission duration, distance from Earth, radiation exposure, mental/behavior analysis, and criticality of individual crewmember functions (pilot, EVAs, robotic operations, spaceflight participant, etc.).]
3.3 Pre-mission Preventive Health Care
[V1 3002] Pre-mission preventive strategies shall be used to reduce in-mission and long-term health medical risks, including, but not limited to:
- Optimization of nutrition.
- Vitamin D supplementation.
- Assessment of medications needed for in-flight use.
- Triennial imaging of bone mineral density.
- Maintenance of optimal aerobic and strength physical fitness.
- Maintenance of flexibility, agility, and balance.
- Annual and pre-flight physicals/periodic health evaluations.
- Preventive dental care.
- Vaccinations as recommended by CDC and local epidemiological conditions as recommended by flight medicine team (e.g., influenza, tetanus toxoid, varicella zoster vaccine, severe acute respiratory syndrome (SARS), coronavirus (COVID-19), etc.).
- Behavioral health and performance training.
- Flight surgeon monitoring of crewmembers during hazardous training and pre-flight science testing.
- Total radiation dose control/monitoring.
- Pre-mission Health-Stabilization Program (HSP) to reduce the likelihood of contracting an infectious disease before launch.
- Assisted Reproductive Technology (ART) if desired by the crewmember to preserve gametocytes prior to missions with exposure to radiation.
[Rationale: Preventive health care tests, procedures, and interventions are required to ensure health pre-mission, during the mission, as well as for the post-mission lifetime of the crewmember. The longer the mission and the farther from Earth (and therefore from definitive care), the greater the extent of preventive interventions that will need to be implemented. Preventive care starts at selection and continues throughout the crewmember’s career, including during missions.]
3.4 In-Mission Preventive Health Care
[V1 3003] All programs shall provide training, in-mission capabilities, and resources to monitor physiological and psychosocial well-being and enable delivery of in-mission preventive health care, based on epidemiological evidence-based probabilistic risk assessment (PRA), individual crewmember needs, clinical practice guidelines, flight surgeon expertise, historical review, mission parameters, and vehicle-derived limitations. These analyses consider the needs and limitations of each specific vehicle and design reference mission (DRM) with particular attention to parameters such as mission duration, expected return time to Earth, mission route and destination, expected radiation profile, concept of operations, and more. In-mission preventive care includes, but is not limited to:
- Periodic monitoring of general health status.
- Optimization and periodic monitoring of nutrition intake – To include caloric density and macro/micronutrients (including antioxidants, flavonoids, lycopene, omega-3 fatty acids, lutein, sterols, and prebiotics), to support multiple physiological systems such as immune function, bone and muscle health, effectiveness of radiation damage repair mechanisms, cognitive and mental well-being, microbiome, etc. Optimization of nutrition intake also includes aspects such as food palatability and food variety to support psychological well-being and crew morale.
- Vitamin D supplementation – For bone and immune function.
- Maintenance and periodic monitoring of aerobic and strength physical fitness – For maintenance of muscle strength and aerobic capacity (essential for performance of safety-critical physical tasks such as emergency vehicle egress), bone strength, cardiovascular health, immune system performance, sensorimotor function, behavioral health/stress relief, and reduction in renal stone formation.
- Maintenance and periodic monitoring of flexibility, agility, and balance – For sensorimotor function (essential for performance of safety-critical physical tasks such as emergency vehicle egress).
- Maintenance and monitoring of work/rest schedules and optimal sleep/circadian rhythm.
- Maintenance and monitoring of environmental parameters at optimal levels for crew health and performance, as outlined in other technical requirements.
- Prevention of pressure-related illness or injury (dysbarism) by utilizing the appropriate prebreathe and equipment protocols.
- Preventive dental care.
- Hearing conservation and protection (as required in [V2 9057] Hearing Protection Provision), including periodic monitoring.
- Optimization and periodic monitoring of psychosocial countermeasures for team cohesion, privacy, social isolation, and sensory deprivation.
- Preventive measures for orthostatic intolerance and neuro-vestibular challenges during G-transitions and adaptation to a new gravity environment.
- Spaceflight Associated Neuro-Ocular Syndrome (SANS) periodic monitoring, and prevention with to-be-determined countermeasures (to be validated by research in the coming years).
- Periodic monitoring of vascular motility and patency of venous drainage pathways in the neck as well as deep veins in the lower extremities.
- Optimization and periodic monitoring of immune function via implementation of a suite of multi-component countermeasures.
- For missions that land on planetary bodies – Training, capabilities, and resources for rehabilitation on the planetary surface, analogous to the functions of the post-Earth-landing recovery team, rehabilitation team, and flight surgeon team to enable surface mission success.
- Monitoring and management of any future risks as they emerge.
[Rationale: In-mission preventive medical care, health care tests, procedures, and interventions are required to ensure and maintain health throughout the mission. The term “in-mission” covers all phases of the mission, from launch, through landing on a planetary body and all surface activities entailed, up to landing back on Earth. In-mission capabilities will vary by vehicle mass, volume, and power limitations and DRM considerations, thus in-mission preventive healthcare is to be tailored to specific mission needs and will subsequently affect risk assessment and pre-mission preventive care accordingly. For an overview of the PRA process and a representative (nonexhaustive) list of medical conditions considered of either high-likelihood or high-consequence for spaceflight missions, please see Appendix E, Table E.2-1—Sample IMM Output.]
3.5 In-Mission Medical Care
[V1 3004] All programs shall provide training, in-mission medical capabilities, and resources to diagnose and treat potential medical conditions based on epidemiological evidence-based PRA, individual crewmember needs, clinical practice guidelines, flight surgeon expertise, historical review, mission parameters, and vehicle-derived limitations. These analyses consider the needs and limitations of each specific vehicle and design reference mission (DRM) with particular attention to parameters such as mission duration, expected return time to Earth, mission route and destination, expected radiation profile, concept of operations, and more. In-mission ctapabilities (including hardware and software), resources (including consumables), and training to enable in-mission medical care, and behavioral care, are to include, but are not limited to:
- Medical system architecture and infrastructure (i.e., electronic medical records (including data encryption/protection), inventory monitoring/maintenance, medical stowage allocation (including pressurized or refrigerated volume), etc.).
- Medical kits (personal, routine, emergency, and survival) and resources, including appropriate pharmaceuticals, equipment, and supplies selected for ease-of-use, and personal protective equipment (e.g., biohazards and sharps containment).
- Configuring environment for medical care (including privacy considerations).
- Obtaining and recording history of medical encounters.
- Performing and recording the physical exam.
- Periodic monitoring and treatment of dental health as appropriate.
- Capability to provide deployed crewmembers with optical correction (e.g., glasses) with increased levels of power to mitigate SANS-induced changes in refractive error.
- Assessing, recording, monitoring, and trending vital signs and additional physiological and behavioral health signs. i. Conducting ancillary tests as needed, including imaging (e.g., cardiac, vascular, ocular), laboratory analyses, and electrocardiography
- Conducting ancillary tests as needed, including imaging (e.g., cardiac, vascular, ocular), laboratory analyses, and electrocardiography.
- Performing procedures and recording outcomes.
- Providing physical restraints for the patient, caregiver, and medical equipment appropriate to specific gravity environments of the mission con-ops.
- Recording treatment plans and its execution as appropriate. m. Administering and managing all medications.
- Administering and managing all medications.
- Consumables.
- Capability to diagnose and treat pressure related illness or injury (dysbarism).
- Monitoring and balancing work/rest schedule.
- Treating neurobehavioral disorders with medical devices and/or evidence-based asynchronous behavioral health treatment protocols available on electronic devices.
- Private two-way communication (e.g., audio, video, messaging, images) with ground medical and psychological support, family, and crew support system.
- Private transmission of medical data (including imaging) to ground medical support or other mission vehicles.
- Means of providing autonomous medical care and advanced life support.
- Medical evacuation.
- Palliative care.
[Rationale: Aspects to be considered in the PRA include, but are not limited to: Mission duration, destination, return-to-Earth capability, mission architecture, spacecraft design, launch/landing loads, crew selection standards, the program’s Health Stabilization Program (HSP), and the need for autonomous-from-Earth medical capabilities. In-mission medical care will be in accordance with current U.S. medical care practices with limitations as imposed by mission constraints and managed by the Flight Surgeon, Deputy Flight Surgeon, or their designees. The term “in-mission” covers all phases of the mission, from launch, through landing on a planetary body and all surface activities entailed, up to landing back on Earth. As each mission may be comprised of consecutive phases that occur in different vehicles, take place in different locations in space with varying distances from Earth, and last for different durations, coordination of onboard medical resources occurs between the medical providers of the different vehicles to ascertain comprehensive care capabilities that allow a successful mission from start to finish.
Medication and supplies are designed to treat the most likely and most impactful medical issues encountered on each DRM/vehicle while abiding by factors including but not limited to storage, vehicle or suited environment, weight/volume, and expiration date. Medications are stored to be accessible and used in a timely fashion. Considerations for medications to be used while a crewmember is suited will need to be assessed for use related to [V2 11027] Suited Medication Administration. All standard medical and survival kits are evaluated per Safety requirements including pharmaceuticals off-gassing toxicity (for example SSP-51721 ISS Safety Requirements Document). Crew specific medical kits are packaged for each individual crewmember based on their medical needs.
For an overview of the PRA process and a representative (non-exhaustive) list of medical conditions considered of either high-likelihood or high-consequence for spaceflight missions, please see Appendix E, Table E.2-1—Sample IMM Output.]
3.6 Medical Evacuation
[V1 3007] Medical evacuation to a location with a higher level of medical care shall be available for illness/injuries occurring during a spaceflight mission which are beyond the medical capabilities available at the crew’s location.
[Rationale: This might entail evacuation to planetary or orbiting assets, or back to Earth, depending on the scenario, medical needs, and availability of resources at each location. The limitations of onboard medical capabilities (including trained medical professionals) means that some illnesses or injuries may require medical interventions beyond those which can be provided during the mission. Assuming a guiding philosophy that preservation of life supersedes preservation of the mission, such severe medical occurrences will necessitate aborting the mission and returning the ill or injured crewmember to Earth for definitive medical care. Depending on mission parameters and orbital dynamics, a return to Earth may not be possible, or may take such a long time as to be rendered futile. In other cases, higher medical capability may be available on a closer-than-Earth asset, either in orbit or on a planetary surface and may be used as a temporizing measure before returning to Earth, or as the location of definitive care.]
3.7 In-Mission Evacuation to definitive Medical Care Facilities
[V1 3008] Plans and vehicle(s) shall be available to transport severely ill or injured crewmember(s) to appropriate Medical Care Facilities, including Definitive Medical Care Facilities (DMCF) in the event of a contingency scenario.
[Rationale: If a return to Earth of a severely ill or injured crewmember is possible and is undertaken, coordination with suitable DMCFs in proximity to potential landing sites will be made in advance of the crewmember’s landing to ascertain readiness of the facility to accept and NASA-STD-3001, VOLUME 1, REVISION C 23 of 86 implement immediate medical care. Mobile ground resources with the capability to initiate medical care enroute to the DMCF will be deployed at potential landing sites.]
3.8 Palliative Comfort care
[V1 3009] The program shall provide in-mission palliative comfort care capabilities for medical scenarios where onboard medical resources have been exhausted, or a timely return to Earth (or another location of higher medical capability) is not feasible, and survival of the crewmember has been determined to be impossible.
[Rationale: Certain medical conditions may occur during a spaceflight mission for which treatment was not manifested, either because those conditions were considered unlikely to occur or were considered to require care beyond that which is feasible for such a mission. If a crewmember were to experience such an illness or traumatic injury for which therapeutic care is not available, palliative care is provided to relieve pain, anxiety, and other types of discomfort. The main medical conditions which have the potential to require palliative care include, but are not limited to, severe trauma, abdominal injury, severe burns, head injury, neck injury, cardiogenic shock, hypovolemic shock, neurogenic shock, radiation sickness, and sepsis. Palliative comfort care may include administration of long-acting analgesics, antiemetics, supplemental oxygen, sedation, other symptom management, and psychosocial support (including religious and cultural if requested) from the ground for the ill or injured crewmember as well as for the rest of the crew.]
3.9 Termination of Care
[V1 3010] Each human spaceflight program shall have criteria for termination of care available prior to flight.
[Rationale: Several medical scenarios could conceivably end with a decision to terminate medical care. Catastrophic injury or very severe illness could be such that either the resources required to sustain life or definitively treat are not available or have been depleted, and/or the medical training of the medical care provider could be insufficient to support such critical and complex medical care. In these rare scenarios, medical care that had begun may need to be withdrawn and palliative comfort care provided, either because of the extreme futility of the situation, because all relevant medical resources have been used and are no longer available, or because continuation of futile measures will completely deplete medical resources and could compromise the survival of the remaining crew if the mission cannot be aborted and medical resources will be needed later on in the mission. The ethical and moral implications of a decision to terminate care are complex and will impact both the surviving crew and the assigned flight surgeons. Policy, procedures, and training prior to flight may be helpful in preparing for such scenarios.]
3.10 Crewmember Mortality
Requirement [V1 3011] updated into [V1 3050], [V1 3051], [V1 3052], [V1 3053], [V1 3054], [V1 3055], [V1 3056].
Despite screening, health care measures, onboard medical interventions, and safety precautions including engineering controls, it is possible for crewmembers to die during a mission, particularly on extended duration missions. Problems that can threaten the health and safety of remaining crewmembers include trauma, grief, mission delays, and contamination. Facilities and plans for handling deceased crewmembers that are socially, psychologically, biologically, culturally, and physically acceptable are to be established during system development. The plan needs to consider the following factors: minimizing risk to surviving crewmembers, potential forensics collection, biohazard containment (via pressurized suit or human remains containment unit), remains return or in-situ disposition, investigation plan, psychological support plan, and legal jurisdiction which will involve working with other federal agencies (such as the Federal Bureau of Investigation) and international partners (via treaties).
3.10.1 Pre-Mission Crew Morality Plan
[V1 3050] The program shall develop and execute a Crew Mortality Plan and determine legal jurisdiction prior to each mission (including pre-flight activities, launch, operations, and landing).
[Rationale: The plan will need to consider individual crewmember desires, including cultural and religious preferences (e.g., is autopsy permissible, what death rituals are to be performed) respectful handling and containment of remains, federal (e.g., Federal Bureau Investigation, Federal Aviation Administration, Space Force, Armed Forces Medical Examiner, National Transportation and Safety Board, Department of Defense, etc.) and international agencies’ requirements (if applicable). This is to ensure proper handling of the remains and the reporting of events is executed in alignment with cultural practices and legal technical requirements. The plan will need to consider all procedures involved during the postmortem process. For in situ burial or jettison of a body into space, shrouding remains will also need to be considered where possible to prevent additional distress to surviving crew/kin by remote imagery collection or distribution. A criminal investigation will take place if deemed necessary by the circumstances of the death.]
3.10.2 Pronouncement of Crew Death
[V1 3051] The program shall define the process to medically assess the death of an in-mission crewmember and legally record the pronouncement of death.
[Rationale: Assessment of death requires the medical capability to assess the crewmember and legally record the death per any state, federal, or international regulations. In some instances, causes of death will be approximated, as the cause and manner of death may be determined without an autopsy examination. Jurisdiction and the process for implementation are to be established in the Crew Mortality Plan prior to the mission and factor in remote mission operations that may impede or prevent direct medical assessment of the deceased crewmember.]
3.10.3 In-Mission Forensic Sample Collection
[V1 3052] The program shall have the capability to obtain in-mission forensic evidence from a deceased crewmember and return this evidence to Earth.
[Rationale: Forensic samples and evidence are desired to understand the circumstances surrounding a fatal event. The forensic evidence (which may include biological sampling, environmental data and/or sampling, operational parameters, etc.) and medicolegal authority for collection and storage of such evidence will be determined in the Crew Mortality Plan prior to each mission. This will include pre-mission coordination with crewmembers and families, federal agencies, and international partners. Implementation of forensic sampling or data collection by surviving crew in-mission will have a clear purpose associated with the event investigation and necessary detail of cause, and not put surviving crew at increased risk of physical or psychological harm. Prior to initiating forensic sampling, continuous assessment of the psychological suitability and willingness of the surviving crewmembers to participate would be conducted such that sampling procedures are terminated at any time that a surviving crewmember is deemed unfit or unwilling to continue. Vehicle design and capability considerations related to the disposition of the crewmember remains will need to meet the requirement as referenced in [V2 6061] Environment Cross-Contamination.]
3.10.4 Crew Morality Remains Return to Earth
[V1 3053] The program shall be capable of returning the remains of a deceased crewmember back to Earth.
[Rationale: Return of the remains of a deceased crewmember is of high priority, however, return of the remains of a crewmember who dies in-mission are not to jeopardize the safe return and psychological wellbeing of surviving crewmembers. Containment of remains considers the length of time a body can be kept in a suit or human remains pouch for each mission. Return will require the ability to control the remains in a sealed or temperature-controlled environment for the period of time necessary to return to Earth. Ability to transport the remains into a vehicle without injury to surviving crew, as well as within the vehicle during return to Earth are to also be considered. Vehicle design and capability considerations related to the disposition of the crewmember remains will need to meet the requirement as referenced in [V2 6061] Environment Cross-Contamination and consider natural processes such as rigor mortis that may set in within hours and last a few days, which may delay or prevent containment, transport, or restraint of remains. Also, reference [V1 3055] Surviving Crew Support for considerations on behavioral health when returning remains.]
3.10.5 In Situ Disposition of Deceased Crewmember Remains
[V1 3054] The program shall meet planetary protection regulations in the case of in situ or jettison disposition of the remains of a deceased crewmember.
[Rationale: Returning the remains of a crewmember who dies in-mission may not be desired due to cultural reasons or be feasible due to risk to other crewmembers (potential toxicological exposures, disease exposure, psychological harm, etc.) or mission circumstances (inability of vehicle or transit duration to accommodate return, inability to extract crewmembers from surface location, etc.). Leaving the remains in situ are to consider planetary protection regulations as well as cultural and technical requirements. This information can be found in the Committee for Space Research (COSPAR) Policy for Planetary Protection, an accepted approach for complying with the Treaty on Principles Governing the Activities of States in the Exploration and Use of Outer Space, including the Moon and Other Celestial Bodies (UN, 1967), Article IX. Additionally, planetary protection categories and guidance to determine the applicability and extent of planetary protection measures for extraterrestrial environments as well as for return to Earth are documented in NPD 8020.7, Biological Contamination Control for Outbound and Inbound Planetary Spacecraft, and NID 8715.129 (or superseding documents) for the Moon and Mars. Vehicle design and capability considerations related to the disposition of the crewmember remains will need to meet the requirement as referenced in [V2 6061] Environment Cross-Contamination.]
3.10.6 Surviving Crew Support
[V1 3055] The program shall provide behavioral health support to the deceased crewmember’s family, surviving crewmembers, and support team in-mission and post-mission.
[Rationale: The program will develop an integrated (including all agencies involved) behavioral health contingency response protocol that identifies and manages adverse behavioral health impacts in affected members in order to meet cultural and organizational needs. Common elements of the contingency response will include, but are not limited to:
- Coordinating extra Private Psychological Conferences (PPCs), either individually or as a group. PPCs will provide surviving crewmembers psychoeducation on grief and trauma reactions, conduct an assessment of psychological functioning, and identify needs for support (i.e., communication with support system, scheduling follow-up PPCs, management of crew time/tasks.
- Coordinating Private Family Conferences (PFCs) for surviving crewmembers.
- Providing counseling/support to crewmember families.
- Consultation and collaboration with the NASA and International Partner (IP) Psychologists and Psychiatrists on how to best support crewmembers and their families.
- Delivery of grief process briefs to impacted groups (e.g., crewmembers, crewmember families, flight surgeons, ground operations personnel).
- Post-mission debriefs to monitor for delayed onset of mental health issues.
Loss of a crewmember in-mission will significantly impact the surviving members and support team (i.e., ground support), both in-mission and post-mission. Surviving crewmembers’ excessive exposure and manipulation of the deceased crewmember’s body during the forensic sampling process increases the risk of acute or delayed mental health injury. This risk is compounded with non-medical crew performing invasive procedures on a close friend or colleague. Assessment of behavioral health in-mission may also drive decision making associated with forensic sample collection and whether to return remains to Earth.]
3.10.7 Crew Morality Mishap Investigation Plan
[V1 3056] The program shall have plans in place prior to a mission to gather the appropriate data to support a Presidential Commission mishap investigation.
[Rationale: The NASA Authorization Act of 2005 (Public Law 109-155, Section 821) mandates that any vehicular disaster involving significant injury or loss of life to onboard NASA crewmembers establishes a Presidential Commission, with federal oversight of mishap response and investigation. Refer to NPR 8621.1, NASA Procedural Technical requirements for Mishap and Close Call Reporting, Investigating, and Recordkeeping for further guidance.]
3.11 Terrestrial Launch/Landing Medical Support
[V1 3012] All programs shall have medical capability at the site of terrestrial launch and landing to address nominal operations and launch/landing contingencies, including, but not limited to the following:
- HSP technical requirements for the crew, the crew’s family, and supporting personnel for purpose of disease prevention.
- Access to the full spectrum of medical capabilities, from routine medical and behavioral health care to advanced trauma life support (ATLS) capabilities, advanced cardiac life support (ACLS), or equivalent.
- Incorporation of civilian and/or Department of Defense (DOD) facilities and Emergency Medical Services (EMS).
[Rationale: Medical support for terrestrial launch and landing needs to consider the local geographic conditions. Technical requirements are provided in the Program Medical Operations Requirements Document (MORD) or similar document and in a Program Technical Requirements Document (PRD) or similar document to task outside agencies for EMS support and ensure its implementation. Medical support at all primary landing sites is to be sufficiently uniform, without disparity between standards of care. If there is no Definitive Medical Care Facility that satisfies the technical requirement for high-quality emergency treatment, mobile or fixed medical suites onsite are to be provided or engaged to protect crew health and afford the capability of resuscitation.]
3.12 Terrestrial Launch/Landing – Definitive Medical Care Facility (DMCF)
3.12.1 DMCF Medical Care
[V1 3013] The program shall establish medical care agreements with DMCF(s) for each launch and landing (nominal and contingency) location.
[Rationale: It is critical to have pre-established medical care agreements with at least one DMCF for each launch and landing location to ensure timely access to appropriate medical care for crew and ground support personnel.]
3.12.2 DMCF Transport
[V1 3014] The program shall have the capability to transport crewmembers to a DMCF for each launch and landing (nominal and contingency) location.
[Rationale: Depending on the location of the launch/landing contingency, transport capabilities may involve evacuation via ground, water, or air by prepositioned civilian and/or DOD assets. All rescue vehicles are to have ATLS or equivalent capabilities to sustain the crewmember until transfer to a DMCF.]
3.13 Certification of Training Plans for Launch/Landing Medical Team
[V1 3015] The organization responsible for crewmember health shall certify training plans for internal NASA medical support personnel who work launch/landing and concur on training plans for external organizations that have a specific medical support training plan in support of a NASA spaceflight program. Training includes, but is not limited to:
- Physiological changes occurring as a result of prolonged launch body posture.
- Spaceflight physiology.
- Injuries resulting from launch and landing contingencies (such as trauma, burns, hypoxia, and hypothermia).
- Hazards of exposure to space vehicle-associated toxic chemicals such as propellant, fuels, oxidizers, thermal control fluids, off-gassed products, and their unique treatments and responses.
- Launch/landing suit, helmet, and equipment configuration and safe removal.
- Vehicle-specific failure modes and resulting injury profiles.
- Environmental considerations specific to nominal and off-nominal recovery conditions.
[Rationale: General medical support training including specific training to prepare the medical support providers to work at a launch/landing site and provide care to crewmembers.]
3.14 Post-Mission Health Care
[V1 3016] Post-mission health care shall be provided to minimize occurrence of deconditioningrelated illness or injury, including but not limited to:
- Physical examinations by a flight surgeon or designated medical support personnel immediately following landing and periodically thereafter, until crewmember status is stable.
- Clinical laboratory tests including but not limited to imaging.
- Physical reconditioning (see [V1 3017] Post-Mission Reconditioning).
- Treatment as required.
- Scheduled days off and rest periods.
- Circadian rhythm entrainment.
- Nutrition assessment and support.
- Behavioral health support for the crewmember and their families to assist with transition back into work and family life.
- Monitoring by a flight surgeon during post-mission scientific investigations that may pose some risk to a deconditioned crewmember’s health.
[Rationale: Post-Mission health care tests, procedures, and interventions are required to reduce risk of deconditioning injury or illness to ensure the post-mission health of the crewmember. This may include but is not limited to physical deconditioning, immunosuppression/risk of infection, and physiological and psychological needs of the crewmember during transition back to terrestrial life.]
3.15 Post-Mission Reconditioning
[V1 3017] All programs shall provide the planning, coordination, and resources for an individualized post-mission reconditioning program, specific to each crewmember, mission type, and mission duration. The post-mission reconditioning starts with crew egress at landing and includes a guided, phased reconditioning protocol. The goals of the reconditioning program include the following:
- To ensure the health and safety of returning crew.
- To actively assist the crew’s return to full functional abilities and return-to-flight status.
- To actively assist in the crew’s return to pre-mission fitness
[Rationale: Post-Mission reconditioning is provided to reduce the risk of deconditioning, injury, or illness and to ensure the post-mission health of the crewmember.]
3.16 Post-Mission Long-Term Monitoring
[V1 3018] Crewmembers returning from spaceflight shall be monitored longitudinally for health, behavioral health, and well-being parameters in a standardized manner.
[Rationale: Data derived from standardized testing procedures, used in a pooled, non-attributable fashion, are essential to characterize the short and (in particular) the long-term effects of spaceflight on human health (occupational surveillance). Exposure metadata from flight monitoring is a critical component correlating exposure to health outcomes and it is important to make such data accessible.]