From Earth orbit to the Moon and Mars, explore the world of human spaceflight with NASA each week on the official podcast of the Johnson Space Center in Houston, Texas. Listen to in-depth conversations with the astronauts, scientists and engineers who make it possible.
On episode 339, a payload developer and surgeon discuss testing a robotic surgery technology demonstration aboard the International Space Station. This episode was recorded on April 10, 2024.

Transcript
Host (Kenna Pell): Houston, we have a podcast! Welcome to the official podcast, the NASA Johnson Space Center, Episode 339, “Robotic Surgery in Space.” I’m Kenna Pell and I’ll be your host today. On this podcast, we bring in the experts, scientists, engineers, and astronauts, all to let you know what’s going on in the world of human spaceflight and more. The Robotic Surgery Test Demo tested the performance of a small robot that was remotely controlled from Earth and performed surgical procedures aboard the International Space Station. In this episode, we had the opportunity to talk with both the developer of the investigation, Shane Farritor, and Dr. Ted Voloyiannis, one of the surgeons that actually operated the robot on station from the ground, carrying out a simulated surgery successfully. So how can remote surgery help folks here on Earth? How can this research prepare humans for future space missions? And what were the time delays like from space to ground? Find out from the experts here for yourself. Let’s dive in to learn more about the first surgical robot aboard the space station.
[Music]
Host: Shane, Ted, thank you for joining us today.
Shane Farritor: Thank you.
Theodoros Voloyiannis: Thank you.
Host: We are here talking about the first surgical robot aboard the International Space Station, and here with some of the folks that made it happen. It launched just at the beginning of this year on January 30 from Cape Canaveral Space Force Station in Florida, onboard a SpaceX Falcon 9 Rocket in Northrop Grumman’s Cygnus spacecraft. So first thing I’d like to ask, how was launch? Were either of you there?
Shane Farritor: I did attend the launch and it was spectacular. You know, it’s great to be at KSC for any reason, but launches are special and watching that first stage booster come back is pretty, pretty spectacular.
Theodoros Voloyiannis: I watched it from Houston online. I had to be in the operating room, so I hope I go next time. But I’m next to NASA here, so it was very exciting to participate remotely.
Host: Yeah, I was going to say, Ted is from Space City, so he knows all about things. NASA over here. And then Shane, you were actually there for the launch, but I don’t think that was your first one, was it?
Shane Farritor: I’ve seen a couple launches before, and on this trip we got to see two Falcon 9 launches. But again, every one’s special and every one’s spectacular.
Host: Absolutely. Well, while launch was exciting, I know that the surgery demo day was likely even more exciting for you all. So more on that soon. But first I want our listeners to get to know you all. So Shane, first, what do you do? Can you explain your job or what you do on the day-to-day?
Shane Farritor: Yeah. I am a robot guy is probably the quickest summary. I’m a mechanical engineer. I’m a professor at the University of Nebraska and I also serve as the Chief Technical Officer for a startup company called Virtual Incision, that’s creating these small robots for surgery called MIRA. But I’m from Nebraska, undergraduate at Nebraska, Master’s and PhD from MIT, and that’s where I started doing Mars rovers. Early in my career, I worked on Mars rovers. I’m mostly now work in surgical robotics. Really happy to get back into the space aspect of this.
Host: Were there a lot of opportunities at University of Nebraska in your undergrad for space? Or maybe you discovered it when you were at MIT?
Shane Farritor: Actually, at the University of Nebraska, I got two internships. I went to Kennedy and worked for a summer. And then I was a co-op student at Goddard Space Flight Center. And then with that experience, in my graduate work at MIT, I was able to participate in some Mars rover work and spent almost a year at the Jet Propulsion Laboratory working on my PhD. So I’ve done a quite a bit of NASA work over the years. And then our surgical robotics were also sponsored by NASA because we make these small robots that can be used in crazy places like the space station. We were sponsored by NASA, cause NASA wants to do surgery in crazy places. So always kind of had a one foot in the space business.
Host: That’s awesome. I was going to ask if you had made it over to JPL too, talking robots and Perseverance and being over at Kennedy and Goddard as well. Now you are the robot guy. Ted, who are you? What’s your version of robot guy? What do you do on the day-to-day?
Theodoros Voloyiannis: I’m the crane operator. I’m the clinician. Basically, I’m surgeon. So I come from Greece from a city named Thessaloniki. I came to Houston and I still live here since 1999. I entered med school in Greece and completed there, but I did my surgery residency in general surgery in Baylor College of Medicine in Houston, and subsequently did my fellowship in colorectal surgery again in Houston. And I practice now almost 18 years. I have a strong interest in advanced minimally invasive surgery since the beginning of my career. At the time, the surgeons used to perform the procedures through a big midline incision, and the majority of the surgeries were performing that way. I had an interesting laparoscopic, minimally invasive surgery through a camera, funny stories that I had a very large hand and couldn’t put my hand through the abdomen when we were doing pancit laparoscopy. And I progressed to develop the multi-port laparoscopic surgery, and soon later, the single incision, only one entry, laparoscopic entrance into the abdomen. And I performed that ever since 2010, almost 2000 of those abdominal surgeries.
Somehow, my path met with Virtual Incision and Shane, who actually developing the same concept for robotic surgery that I perform, at the same time I’m serving as a chairman of the U.S. Oncology Network for colorectal surgery. And I’m one of the surgeons in nationally that assess hospital systems for accreditation for rectal cancer, which is my need. I perform all my procedures here in Houston. And I also have a very strong interest in public health and helping patients to achieve healthcare in new ways and improve our system. And for this, I’m also entering into a master’s program this summer at the Harvard T.H. Chan School to pursue Master in Healthcare Management.
Host: Okay. Just, wow. That was amazing hearing both of y’all. And it’s funny, you know, being here, like I can see both Shane and Ted on the Teams screen here, sorry, on the screen as we’re talking. And you’ve got Ted and his scrubs, and then you’ve got Shane with his spaceMIRA Virtual Incision screen in the background. So it’s funny to see sort of the both and with your specialties there. So I think it probably at this point is obvious to our listeners, but we talked about your day-to-day jobs. What exactly were your roles with spaceMIRA?
Shane Farritor: Well, as I had mentioned before, you know, we’ve been doing research with NASA sponsorship for a long time to create a forward deployable surgical robot. Actually, the Army and NASA both have sponsored our research because they both want to do surgery in crazy places. And so, as we are developing a more and more capable device and started to commercialize that device, we received an award from NASA to fly on the space station because our robot was getting more and more useful, and having a flight mission is a nice sort of capstone to our previous work with NASA. So, you know, we were granted this award and we spent about a year and a half sort of designing the experiment and setting it up. And then, as you mentioned, it flew this January, and in February we did a couple different experiments, which I can tell you about in a bit.
The device is currently up on the space station, and we think towards the end of this month, it’ll be coming back to us. So really successful mission. Honestly, I couldn’t have imagined that it could have gone better. One part of the experiment was to have surgeons on Earth control the device that’s on the space station. So perform some remote simulated surgical tasks from a distance with the idea that you would be moving towards remote surgery or telesurgery. And so we actually had six surgeons involved in that process and was very, very happy that Dr. Voloyiannis participated in that. So, Ted, that probably gets you to your role. Go ahead.
Theodoros Voloyiannis: Yeah. So I met the MIRA team last year, more than a year ago. And we have spent a full day in Lincoln, Nebraska at the lab and got to get introduced to the single incision approach and the concept of developing the smallest size and robotic device, miniature device for a multi-quadrant abdominal surgery. It was right into my niche because I performed these procedures all these years with the same goal, to miniaturize my approach. However, I have used whatever is available on the shelf in terms of technology from the current robotic systems and instruments and available techniques. So I have developed my technique on my own to perform this procedure. But I never found the opportunity to have a company and an engineer behind that to lead this effort to simplify their procedure and potentially apply it to other subspecialties in the surgical world and make it easier to be able to be learned easier and applied by younger surgeons without the need to have any significant training beyond their specialty training that is required. So it was basically love on first sight, I would say when I saw that, I say, “Oh my God, this has the potential to grow.” And my goal, I think my involvement, is to bring all my knowledge and experience from the last 10 years of performing these procedures and improve the technique and perform it in patients here on Earth. And my second will be to participate in the greater goal of developing telesurgery.
Host: Now, Ted, you had mentioned you fell in love with how this wasn’t what we call commercial off-the-shelf. This was sort of a new way to go about it. And when you got involved with Virtual Incision, was that before you even knew about spaceMIRA? It was just MIRA on the ground?
Theodoros Voloyiannis: Yes, it was before that. And that came along the way. Basically, my goal was to develop the technique for colorectal surgery, hoping that at some point, we will obtain FDA authorization for these procedures. And considering colorectal surgery may have a funny name as a specialty, but it’s pretty complicated because it is applied in different quadrants in the abdomen. And developing a robotic system that can actually suit that role is very challenging. So that’s why when I got my hands on it and I did the first simulated surgery in Lincoln on the lab, I said, “Okay, this has the potential to do this.” Of course, the space experiment came later. It’s one of those things that you can never dream of and dream about. And it was even more exciting for me.

Host: Someone not in the medical field, and I found that so fascinating that your specific niche of surgical operations that you do brought you to finding this new instrument and brought you to Nebraska. I was going to ask how did a engineer in Nebraska and a surgeon in Texas work on this together? But Ted, you laid that out so perfect. And it seems like you’ve sort of been there since the beginning. Would you say so, or maybe a few years into when Shane, you were working on this?
Shane Farritor: Well, there was a long period, you know, this has been a long process of developing MIRA and spaceMIRA, over almost 20 years actually. So we actually started doing this research in about 2001. When the idea of robotic surgery was just beginning. 2001 was actually when the first soft tissue robot was approved by the FDA. But I worked with a surgeon named Dmitry Oleynikov here at the University of Nebraska Medical Center. And we both thought that there was this idea of making little robots that go inside of the body rather than big robots on the outside. So that was kind of the core principle that all this is built on, these little robots that actually go inside the body and basically try to shrink the surgeon down and put them in there so they can have direct access to the surgical target. And we’ve been developing this idea for a long time. Again, it was research sponsored by NASA and by the Army over a long time. And honestly, we made a lot of really bad robots. And as a way to figure out what the good robots should look like, we made a lot of bad ones. Of course, early on, the robots looked like rovers cause I was a Mars rover guy. And that was kind of our first direction we went. And then yes, then we eventually got our robot working well, we started going through the approval process with the Food and Drug Administration and we pulled in Dr. Voloyiannis because he’s a sort of a national leader in colorectal surgery. And he already mentioned to you some really innovative approaches to those procedures. So he’s the kind of guy you want to have involved in helping you think through both MIRA and spaceMIRA.
Host: Got it. Now, Ted, as a professional in the medical field and all the way from Greece, did you ever think your work would travel as far as 250 miles above Earth?
Theodoros Voloyiannis: I never thought I would travel 6,200 miles from Greece to Houston, but here I am, so another 250 miles to that, added a little bit to now this was an out of this world for me to say that joke, I felt like…I never thought that I would do this, and I would never felt this is going to be an option in my career, I mean, in the middle of my career. And I never felt that surgery and technology will progress so fast that we would, that we are, every day on the surgical field. We wouldn’t even predict that this will count will come to play and happen. The same way that Shane describes the path of almost 20 years of work. It’s an enormous amount of work and try on narrow until they handed to me on my hand the device last year, it needed 20 years of work behind before that.
Similarly for me, I had done a lot of trial and error in techniques over the past 15 years in developing this procedure for my specialty. The other issue that we have many times in our surgical field is many surgeons say, “If it’s not broken, why you want to fix it?” So it’s very difficult to start an innovative technique where you do things with a big incision or a smaller incision, and now you want to do a tiny miniaturized incision. And sometimes you have to go against the mass of your peers to pursue new technology and new avenues and new techniques at the same time. Sometimes even patients don’t seem at first to acknowledge or recognize the importance of that. When you see someone, for example, with cancer, they will say, “All I care is you take my cancer out. Now how are you going to do it? I don’t care.” But you as a physician, as a clinician, you have to see the big picture and offering them a procedure that will benefit them by offering smaller incision, quicker recovery, and less pain. That’s how I think you see better outcomes. You see them returning to work faster and of course, decreasing the cost in healthcare. So that’s why I think when the miniaturized robotic device comes into play, and that’s how we both met almost after 15, 20 years of each of us in separate experiences and trials and errors to develop this technique together and help this technology improve.
Host: That was a great summary of how you all came together on this. And even more than 20 years or so, I wanted to say that you were totally allowed to say out of this world, it’s so hard not to at times. And so you were totally allowed. If that comes up again, Shane, you too. but Shane, can you tell us about, I guess, a little bit more about the evolution of the spaceMIRA? So you were working EarthMIRA, or just MIRA for short, from the idea to origin to the successful demo on the space station. Can you talk us through that?
Shane Farritor: Yeah, sure. Again, we started in about 2001, me and my co-founder, Dr. Dmitry Oleynikov, making these small robots. And this was really just research inside the university, but it was a special partnership because Dmitry was a clinician and I was an engineer, and we really had a very collaborative, hands-on relationship. And we built a lot of robots. That was kind of our ethos the entire time. We would build a robot and we would test it in surgery and go back and forth and back and forth, you know, multiple times per year. And that led us to a device like we have today that we think is very, very useful in surgery. And so that’s where we reached out to more clinicians like Dr. Voloyiannis. And that early research, again, was of interest in NASA because of the ability to deploy it in remote locations.
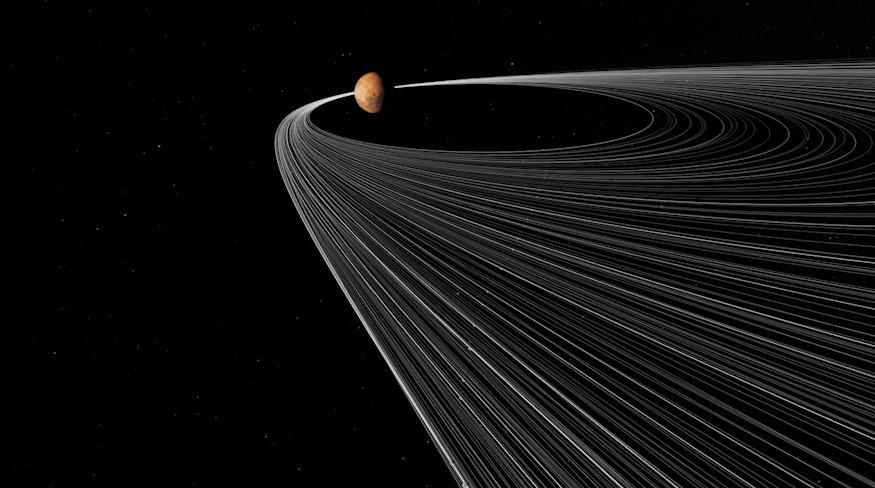
So we proposed the spaceMIRA idea. And that is an excellent example of you know, the idea of telesurgery where a surgeon is at a remote location and operates a deployed device with a patient there and can bring their expertise over the internet to that patient without being physically present. And of course, that has, you know, you start thinking about rural areas in the United States and critical access hospitals and those kind of places where there may not be a colorectal specialist like Dr. Voloyiannis if they can dial in and assist with procedures from a distance. You can talk about the developing world where surgeons are not common, and where one surgeon could do a lot of work from a remote location and help a lot of people that way. And then you can talk about just straight up telesurgery, just improving efficiency by allowing different surgeons, by making independent of their location. So a great way to demonstrate that was with this space station mission. You mentioned it’s 250 miles above the Earth, but it’s also spin around the Earth. So you can get 8,000 miles away very quickly. So we were very happy that we had a group of surgeons. It wasn’t just one expert surgeon; it was a group of surgeons that were able to perform this telesurgery. So I said, it’s very successful. There is some penalty of communication lag in there, but like we say to the space station, all six surgeons were able to accomplish their tasks as required.
Host: So six surgeons on the ground, and you got into this Earth-based, right? So rural areas may not have surgeons available or common. And so it was sort of why sending it to the space station was important for future long-term missions to the Moon and Mars, where surgeons may not be on board there with them. And so something like this could possibly help them in the future there.
Shane Farritor: Yes. And as part of our research, we commonly do these surgeries, simulated surgeries, across, you know, different distances. We do them here in Lincoln, Nebraska, or across Nebraska, across the U.S. We’ve done Johnson Space Center to Omaha, Nebraska, where we had a former astronaut controlling the device from Johnson and the simulated patient was here in Nebraska. We’ve done Honolulu to Nebraska. So we’ve done quite a few of these over the years.
Host: Now I’m curious, is your hope one day to drive the cost of, say, space or Earth or just MIRA down so that these could be deployed to areas that may not have surgeons around or maybe at urgent cares?
Shane Farritor: Yeah, I would push it to say I want patients to have better access to robotic surgical care, better surgical care overall. And that comes in a lot of forms. Price is certainly an issue that complicates things, but it’s also simplicity of use. It’s also geography. There can be a lot of things that factor into getting good quality healthcare access to everyone. And that’s kind of what we’re pushing for.
Host: Sure. Okay. Now let’s talk about the mini robotic surgeon itself. And so Ted, while this section’s a little bit more about the robot’s design, please feel free to chime in cause you’re the one that got to operate it, and I see Shane showing me it in the screen here. That is really cool. First, Shane, the history of the robotic surgeon. So the how and the why it was developed and tested on the ground. I think we went over quite a bit of that. Was there anything you wanted to add there?
Shane Farritor: No, we just go back to this, like I say this principle of little robots that go inside the body rather than big robots on the outside. The devices that are out there and commonly used are generally nine feet tall and weigh a couple thousand pounds. That’s difficult to deploy and certainly has some advantages, but also some drawbacks in terms of complexity and, and getting access to those kinds of machines. So we developed a robot that’s handheld, it’s actually comes out of a surgical tray sterile. So it’s something you can carry around quite easily. And that again, lends itself to crazy locations like NASA is interested in.
Theodoros Voloyiannis: I want to add something on that. That something that sometimes patients don’t realize. A very large robot of the size is very difficult to be deployed in an average hospital. The average hospital operating room is very small in size. So not every operating room can have the regular size robots that we have today. In addition to that, you have to have robotics teams, central supplies. You may have to modify electricals on those rooms. It goes on and on and on, how much it takes to install a robot in a hospital nowadays. And this one is smaller and portable. That’s what I found fascinating. I could see this even going to the surgery centers and it could be used also for outpatient procedures, which can transform completely the way we do surgery today. Everybody thinks surgery has doing it in a hospital. So I feel like there’s a lot of opportunity there because of the miniaturized size and the feasibility in deploying it, and don’t need to have a whole team around it to operate it.
Host: Ted, thanks. There are so many questions to ask about the robot, right? And so I’m asking, you know, Shane, and then you come in with this niche side of things that I would’ve never thought of, right? So robots being too big for an operating room, and there’s already so many in there. That was super interesting. And so, Ted, you’ve worked on this exact robotic assisted surgical device on the ground, right? You’ve worked with MIRA on patients. About how many procedures have you done with MIRA?
Theodoros Voloyiannis: Not on patients. I did animal surgery and laboratory surgery. So I didn’t perform on patients yet. They are about, if I’m correct saying, and correct me, that 15 or 20 procedures before performed on patients for the FDA authorization by my partner and colleague.
Shane Farritor: Yeah. I’ll speak to that. So we just received market authorization from the Food and Drug Administration just in February of this year to market our device. As part of that approval, we did a clinical trial, a very rigorous clinical trial, here in the United States where we had surgeons at three sites perform 30 different procedures. So that’s the human history of MIRA’s development.
Host: Okay. Wow. That’s exciting. And I wanted to know, Shane, how many iterations of MIRA have there been? And you were probably a part of maybe learning and testing on those iterations?
Shane Farritor: Well, how many iterations? Certainly north of a hundred. They weren’t all MIRAs. They weren’t all called MIRAs. That’s a name reserved for our most recent version, one version. But many different types of devices over the years. We’ve built and tested; Ted’s absolutely been involved in that development and has contributed a lot to kind of a lot of the design that you see today.

Theodoros Voloyiannis: Yeah. And then moving forward to improve the single axis. And once you have the one that you saw on the screen today that Shane showed you, this one now is going to become, I would say, more perfected and maybe tailored to different subspecialties, for example, colorectal versus other specialties like gynecology or urology that may have variations of that and in their instruments and the things that they can do.
Host: Okay. And Shane, how did you hear about the opportunity to get MIRA on the ISS and was there a grant involved? Can you walk us through that process?
Shane Farritor: Yeah, there was a grant involved. And again, it started with sort of years of sponsorship of you know, the human spaceflight office at Johnson has been the program management branch for our previous research. And when those grants, you know, kind of came to an end and we really turned our attention to Earth-based activities. This opportunity popped up through the Nebraska Space Grant Consortium and they suggested that we apply for this grant. We had our history with NASA, and it was a good fit for us. So at that same time, we were sort of exploring this idea of telesurgery. And this is absolutely a fantastic way of demonstrating telesurgery. You don’t get much more remote than this International Space Station.
Host: Absolutely. And can you tell us the objectives of the technology demonstration on board the space station?
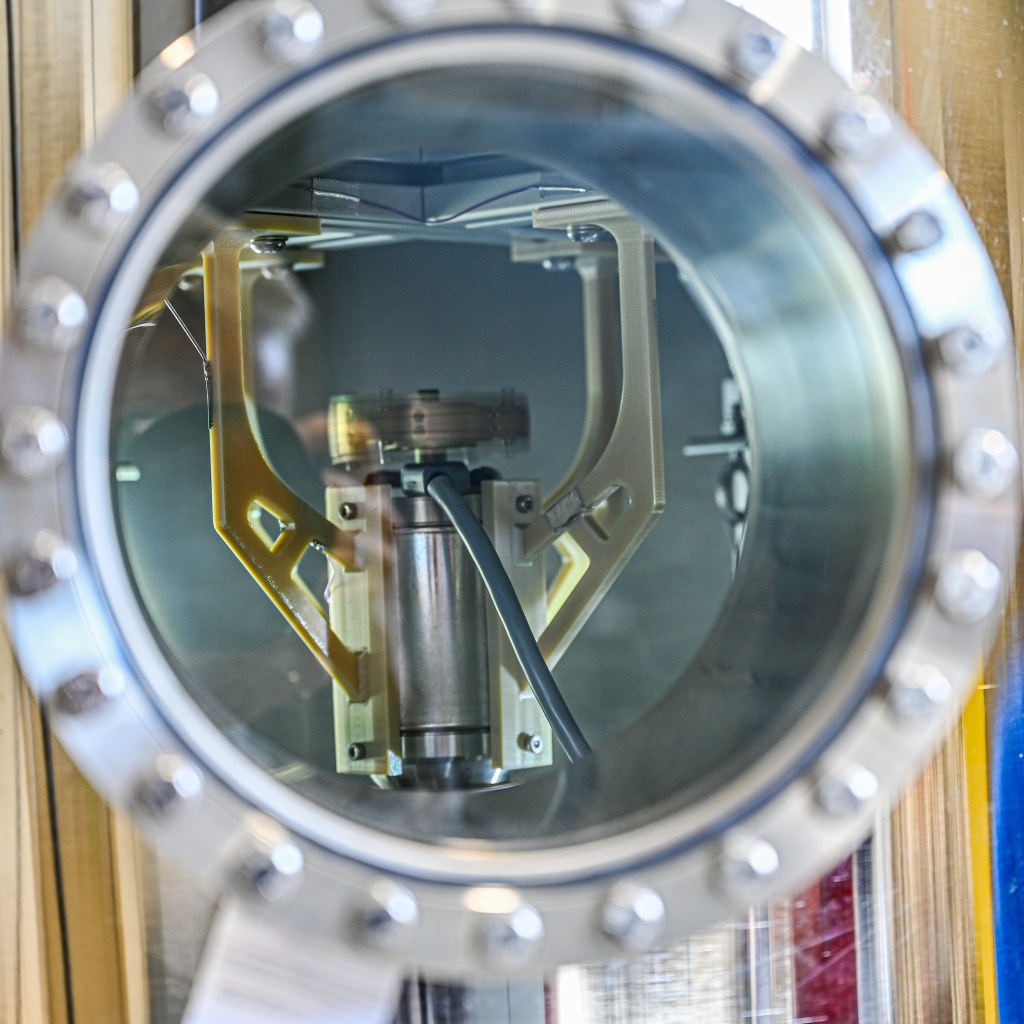
Shane Farritor: Yeah. First of all, I would point out that it was a technology demonstration. We weren’t actually doing surgery. We were sort of doing some simulated surgical tasks, but really the goal was to demonstrate the capabilities of the technology. So what a small robot can do and what can be done with different communication protocols and different latency between the surgeon and the patient. There were really two experiments that we performed. The device was installed inside and of what’s called an Express Rack Locker. And that’s a microwave sized box, that’s a standard experiment box for the space station. It really grew out of the middeck lockers from the Space Shuttle Program, but this microwave sized box was taken off the Cygnus cargo ship, installed into the rack, and the astronaut connected the ethernet and power from the space station to power our device. And really, they just turned it on at that stage. And our first experiment began.
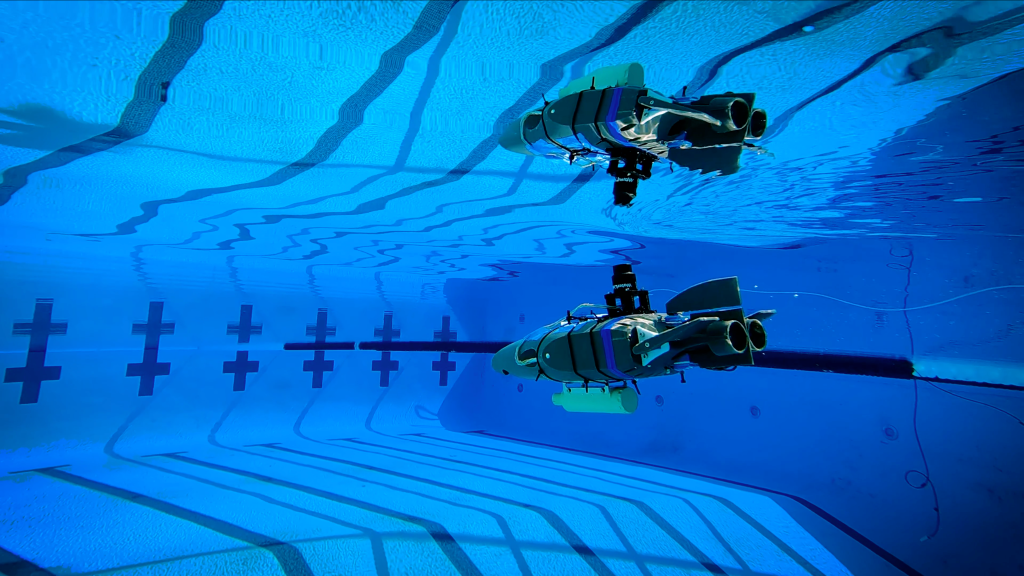
So in the first experiment, the robot went through a pre-program path to perform some simulated surgical tasks. So that was kind of an autonomous mode where robot did it all on its own. We did that experiment first because, you know, it’s not easy to make sure your experiment’s going to work and make sure you can establish the two-way communication required and we wanted to get something on the space station. So that worked out quite well, and that made us feel really good about what was to come. And so we looked at that data for a couple days, and then Dr. Voloyiannis and the other five surgeons came to Lincoln, Nebraska, and we had a second experiment again, where the device was controlled by the surgeons on Earth here in Lincoln. And they performed very similar task stretching and dissecting simulated surgical tissue while the tissue was up on the space station. So both experiments were shockingly successful. I was very excited with both outcomes and can’t wait to get the device back. There’s a little bit more data we can collect from the hardware when it returns to Earth and then we’ll have a lot of great data to analyze.
Host: I have so many questions. And first I want to talk a little bit about maybe the enhancements to the tool and if it looked a little bit different than it does on the ground going to space. Cause like you said, it had to fit into that Express Rack Locker. And so were there any enhancements to make it fit on its ride to station?
Shane Farritor: Yeah, I mean, very slight. Our device’s, you know, about as long as your forearm, I would say, you know, it’s 22 inches, I think long for the Earth-based MIRA. And a lot of that is to fit many different. Ted can speak to this more directly than I can, but people have all kinds of different thicknesses of their abdominal wall. So there’s big people in the world and small people in the world. And so our robot has a section that’s made to accommodate for different thicknesses of the abdominal wall. We didn’t need that space in the spaceMIRA version, so we just shortened that middle section by about three inches. And that was really the only modification we made between spaceMIRA and Earth-based MIRA.
Host: Okay. So no additional really special enhancements to the tool. It was essentially the same thing there, just a little bit shorter to fit in the box, and you just didn’t need that extra little bit there.
Shane Farritor: Exactly right.
Host: Okay. So Shane, I was looking at your bio before this and you can add space-based technology demos and the process of getting them to low Earth orbit now on your area of expertise, working through a launch campaign. Were there any challenges that surprised you in the process of getting it to the space station? Maybe meeting timelines, weight restriction size, stuff like that? I know you’ve worked space stuff before, but was there anything particular with this?
Shane Farritor: No big surprises. What was very different was we had a lot of Zoom meetings. That’s kind of new to all of us in the work world, I guess. But no big surprises. There’s this fair amount of testing and paperwork that goes along with any mission like this. You want to ensure that it’s going to work properly and that you’ve done everything in the right way. But we also do that as part of our regulatory approval here on Earth. So we were pretty used to that process and it went quite smoothly actually. So no big surprises.

Host: Okay. And then now to fast forward to spaceMIRA onboard the space station, I think it was about, was it two months ago to the day that all six of you or the six surgeons, you, Shane, and your team’s were up in Nebraska in what looked like—did you have a sort of mission control going on there?
Shane Farritor: Yeah, we created our own mission control. It was a special occasion for us, and we wanted to do it up properly. So we had a couple of workstations set up for engineers to interact with the device and to communicate with the NASA personnel who communicated with the space station. Then behind that, we had all of our surgeons lined up so that they were ready to go. And then in the front of the room, we had the actual console that would control the device, and then lots of nice big TV screens to display to everyone in the room what was going on. So, yes, we kind of created our own little mission control.
Host: You know what it reminded me of: JPL, or a little bit of Johnson Space Center. I know you’ve been at both, so that was really funny. I liked it. It looked really, really cool. You had mentioned that there was a little bit of setup required before, so the astronaut I’m guessing just sort of inserted the rack and then turned it on and it had the pre-programmed autonomous demonstration that happened a few days before. And then you guys were next. Who was the crew member that helped you? Was it Loral O’Hara?
Shane Farritor: It was. You know, she’s the operator of the Canadarm and the robotics expert that was on board at that time. So we were really lucky to have her involved with our experiments as well.
Host: And she’s here in Houston. Ted, over with us.
Shane Farritor: She’s freshly back. Freshly returned, right?
Host: Yes, she is. Yep. And she’s from this area too. Once she had set it up, how many surgery-like tasks were executed? So she had set it up a few days later. You all were ready. You’re sitting there, you’re talking to Marshall Space Flight Center. Who is involved in, leads sort of the science payloads on station and those executions of that. How many were actually taking place at that time with you all?
Shane Farritor: Well, we had simulated surgical tissue where the surgeon had to grasp tissue at a particular location, provide tension to that tissue, and then they could dissect that simulated tissue. And that’s representative of a lot that happens in surgery. And roughly, there were six surgeons and they performed two or three of these activities each. We had one surgeon that did a little bit more to get a little more depth from one sample. I don’t mean to call surgeon samples, but one experimenter. And then we had the other five did two or three activities as well. Ted, is that roughly correct?
Theodoros Voloyiannis: Yep. Yep.
Host: And Ted, I can’t wait to hear about your experience and what it was like. I have so many questions there, but first I want to know, what was the surface you were working on? Was it supposed to resemble tissue? What did that look like? And did you have to, I guess, insert new “tissue,” or how does that work?

Theodoros Voloyiannis: It is, think about, you know, in the sim the most simplified surgical tasks that you learned since the very first day you go into a surgical program is learning to dissect and cut, and you have to learn precision, accuracy and be able to perform this more maneuvering repetitively with success. It may sound easy, but it may not, it’s not the same like cutting a piece of paper with your scissors at home. So cutting through tissue takes a lot of accuracy. And believe it or not, there are multiple different types of scissors with different names in the surgical field. So to dissect more into this process, the surgical task was basically handling the robotic device remotely. You’ll be able to able to maneuver the arms in the tiny space you have there, which for me was pretty much, I was very familiar with that because single incision laparoscopic and robotic surgery is exactly that.
You’re operating in a very small narrow field right around, think about it, at three to four square inch area where you do the procedure. It’s not like doing open abdominal surgery where you have your hands in there and you’re looking from outside. So that was the easy part for me. Then the actual tissue, the surface, it was elastic bands that they were pretty wide, and it had the relative thickness to simulate thing, stimulate, like cutting, you would say skin or adipose tissue or maybe a capsule of an organ. And they were not so easy to go through. You had to basically hold the appropriate tension and maneuver it properly, and then orient your seizures in related to your grasper and your other hand and perform the cutting. And then of course, the repetition of that was also a factor. And if you add to the lack of the time that we had to send a signal and maybe a little bit of difficulty with the perception of the depth into that environment where the robotic device was installed, that adds a little bit to the difficulty of the procedure.
So to talk a little bit about how I got involved is like when I got a call, you know, with a two, three day notice, “Hey, you’re going to come.” The very first thing you think when you fly there is exactly what the surgeon thinks on Monday morning that you’re going to get a call from the hospital. Your case is canceled for many different reasons. So that call never came, and this was not canceled, and it was everything done perfectly. So we were asked to do through a training first on the console and practice on that. And that’s another thing that sometimes messes up with your brain as a surgeon. You do this simulated task in your console here. And it’s so easy to do. And you say, how come this can go wrong? I mean, I’ve done it a million times, but then once you do it remotely, there it’s a little bit different. And your heart rate is up and the adrenaline is up. But then once you ask the first minutes and you feel like you do it correctly, then you relax and then you feel like you learn doing, you know, biking again. So that’s how I felt.
Host: A surgeon saying it’s like you learn to bike again. Shane, I thought that it was interesting and like all I know is maybe like from watching Grey’s Anatomy, which is bad, but you mentioned scissors and grasper, right? So is that what’s on the left? What’s on the right? Is what you’re sitting at the front of the room resemble what you would be using on Earth anyway with this type of operation?
Shane Farritor: Yeah, it does. And we’ll have Ted comment on this too, but first I need to tell how excited my daughter will be that Grey’s Anatomy came up today. So that’s good. My daughter would be excited about that. So it’s one of the, I think, exciting aspects of our robot is that yes, on that screen you’ll see a grasper on the left side and a pair of scissors on the right on Earth. Both of those would have cautery, which is really high energy electrical signals that will allow the surgeon to burn tissue and cut tissue to prevent bleeding. But the camera importantly is between your two arms. It’s made like you and I are, and in robotic surgery or in what’s called laparoscopic surgery. That’s not always the case. Sometimes your camera will come in from the side, and that can really make it more difficult in the way you move your instruments because it doesn’t match your natural perception. And this principle called triangulation, where you get a right arm and a left arm, and in between that is the third point, which is your visual field. So, one of the advantages of our device is that you always have this very good triangulation, sort of this predator view of your surgical target. So that’s is an important part of what we do and how the experiment was performed. Ted, maybe you have something to add to that?
Theodoros Voloyiannis: Yeah. I agree to this and I felt like the angle of the camera was the most important thing. And I think what you taught me, I remember, which kind of helped me a lot in that moment was to actually look at the shadow of the instrument onto the rubber band. And as we approach it slowly, the thickness of the shadow decreases. And then that’s how you know you’re getting closer to it and you control the movement. Cause remember, you’re doing this with about 0.65, 0.85 of the second of lag. And you execute the move, and then you wait to see what happened. So you have to approach the rubber band, you don’t want to bypass it or go above it or below it. And this little trick helped me a lot to enhance my depth perception.
Host: That’s fascinating.
Shane Farritor: I would add that surgeons like Ted will have all kinds of different skills. But one of them is this ability to measure depth and kind of immerse themselves in a sort of foreign environment, whether that’s surgery on Earth or surgery on the space station. And anyway, we had a great group of surgeons to work with Ted right in there.
Host: And Ted, what you said was fascinating, maybe this was something different on the space station, that it was a little bit challenging, where you had to look at the shadow to see how close you were, versus maybe you wouldn’t be doing that on the ground because you don’t have that delay or that lag. How was that, how was the lag and how was that challenging?
Theodoros Voloyiannis: Honestly, I thought it would be a greater lag than we actually had. We were prepared, I think for closer to the second. But we had times where it was close to 0.65, which fairly feels close to normal, or once it goes up towards .85, you’ve got to wait on your movement. So one of the big rules there is I had to adjust my arm. So any movement I would do, it will produce a very small forward movement with my hand. In other words, I didn’t want to make the wide movements I do on an actual surgery because I had to wait to see what happens first. And think about f you’re doing surgery in the abdomen, everything inside may look pink and yellow, but everything has a name. So you don’t want to hit a vessel, you don’t want to hit a nerve, you don’t want to cause damage into any interabdominal structure. So this really actually the lagging, I would say reminded me of my very first days of training where you were doing the small movements with a lot of accuracy and actually see the result of your task that you just executed. And it makes you feel like, you know, your first years, where you’re very cautious of what you do. And once you get acquainted with it, then after that becomes a little bit more of a normal task.
Host: And what was that feeling like when you successfully carried out the demo?
Theodoros Voloyiannis: I never thought I would be successfully doing something like this. The of this, of the new and the unknown is what gave me that great feel of gratitude and also all this other thoughts about, oh my God, what will be next and how we going to apply that in Earth and all this horizons are opening for us now. I think it’s the beginning of a new era in surgery.
Host: I’m sure there was so much excitement in that mission control University of Nebraska room there. And I want to know, what’s next for spaceMIRA?
Shane Farritor: Well, it’s a good question. What’s next for spaceMIRA, as I mentioned earlier, it’s still up on the space station and will return at the end of this month. And we hope to get the device, you know, a couple weeks after that probably. We have lofty goals in terms of commercializing our technology here on Earth, and, look forward to deploying it and helping some patients with our new device. But we’re certainly going to do research in the area of telesurgery. I hope we could fly again at some point. We’ll see if there are other opportunities that present themselves. But we’re certainly going to start doing telesurgery, hopefully all over the country and eventually all over the world.

Host: And so I know you all will probably want to compare data doing the same tasks on the ground versus what you had done from the ground to space station. Did you already do that, or did you already know, basically with the lag that you expected versus the lag that you did get in command? Was that sort of all the data that you needed to collect or is there more in the future?
Shane Farritor: Well, we’re compiling a lot of that data now. So, Dr. Voloyiannis has used a device on Earth where there’s very minimal lag. And then we trained him with some latency like we expected to see on the space station. And then he actually performed experiments like you see on the space station. And then we have, you know, both breadth and depth. We have six surgeons at the event was sort of our breadth. But then we’ve been working with a couple other surgeons to really try a little bit of lag, a medium amount of lag, and then the space station lag and see how that changes their performance. And I’m eager to, again, collect all this data together and we’ll be processing that over the next coming months and I’m sure we’ll be publishing.
Host: Where is spaceMIRA going to go on display?
[Laughs]
Shane Farritor: Good question. Probably at the Virtual Incision headquarters here in Lincoln, Nebraska. Actually, we’ve been asked to display, display at a museum in Chicago. It’s the Museum of Surgical Science. It’s going to have a display on space medicine. And of course, if you have a museum of surgery along with a display on space medicine, a traveling exhibit on space medicine spaceMIRA, a space surgical robot sort of fits right between those two.
Host: I was going to say.
Shane Farritor: We’re going to take our ground test unit and we’re going to have it on display the last six months of this calendar year in Chicago.
Host: Very cool. Last question for you both. What do you hope the general public takes away from this breakthrough tech demo?
Shane Farritor: I’ll go first. I’m eager to hear what Dr. Voloyiannis has to say. Well, I hope that they realize there are folks out here trying to advance and improve surgery and NASA has a role to play in that. And this idea of telesurgery could be a very positive one. And we hope to impact first hundreds and thousands and ultimately millions of patients worldwide with this new technology.
Theodoros Voloyiannis: I feel like that physicians always trying to find new ways to help patients and achieve better outcomes and find best solutions for their condition. And I’m one of those that since the beginning of my career, always push the boundaries. I wanted to find a better solution for the surgical problems I was dealing with. And I think with this miniaturized robotic device, I have the opportunity to pursue this goal and maybe see results much sooner than I was expecting. The goal would be to improve the way we do surgery in the hospital like we do today. Better, faster, quicker, cheaper, with the same outcomes that we do with the conventional methods we do today. The second option, the second opportunity would be for telesurgery. Approximately 30% of the counties in the United States will not have a surgeon in 10 years. And this is a problem and I think there could be a potential solution with telesurgery and pursuing that. And then the third one could be, in my opinion, training younger surgeons remotely as well, or think about intraoperative consultations by more experienced surgeons to other surgeons in other locations, in other hospitals. So I think there is endless opportunities here for the future by per performing this experiment two months ago today.
Host: And in your words, Ted, it’s a great leap for surgery.
Theodoros Voloyiannis: Yes. That’s right. It was a small rubber band cut, but a great leap for surgery.
Host: I love it. Congratulations on not only the first surgical robot aboard the space station but executing the demos successfully. Thank you both so much for being on the podcast today.
Shane Farritor Thank you, Kenna.
Theodoros Voloyiannis: Thank you so much.
[Music]
Host: Thanks for sticking around. I hope you learned something today. Check out nasa.gov for the latest, nasa.gov/podcasts and check us out on social media at Johnson on Facebook, X, and Instagram. Use #AskNASA on your favorite platform to submit your idea and make sure to mention it’s for Houston we Have a Podcast. This episode was recorded on April 10, 2024. Thanks to Gary Jordan. Will Flato, Dane Turner, Abby Graf, Destiny Duran, Aaron Crowley, Shay Smith, and Dominique Crespo. And of course, thanks again to Shane Farritor and Dr. Ted Voloyiannis for taking the time to come on the show. Give us a rating at feedback on whatever platform you’re listening to us on and tell us what you think of our podcast. We’ll be back next week.
This is an Official NASA Podcast.