Lee esta historia en español aquí.
The human heart takes center stage during the month of February. It is American Heart Month, an effort to raise awareness about heart disease prevention. People also celebrate Valentine’s Day, a focus on the heart’s symbolism in love and friendship.
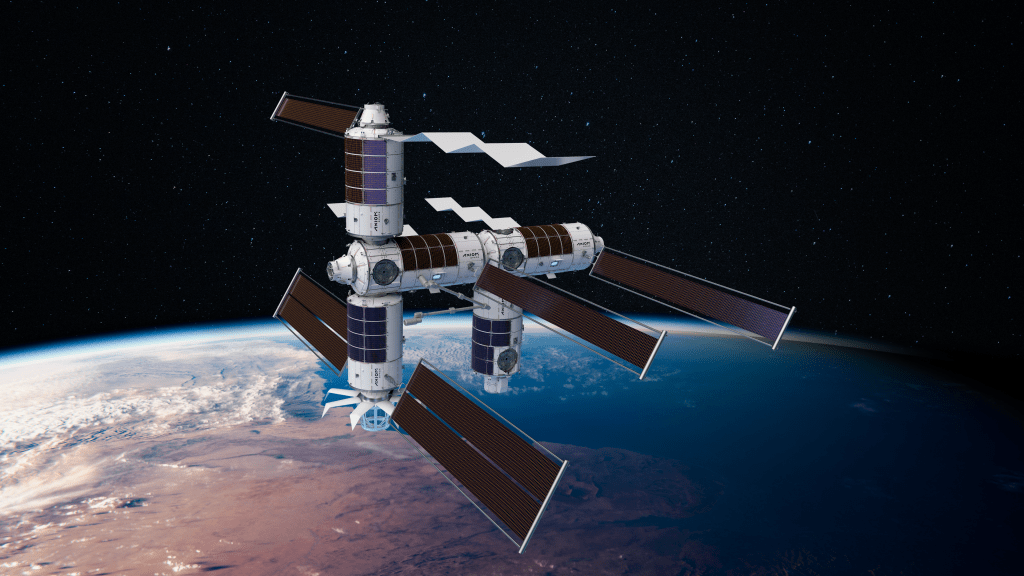
On the International Space Station, the human heart takes center stage year-round. Diseases or other factors like aging that affect the heart can change a person’s overall health and well-being. Microgravity is one of those factors, and recent studies sponsored by the ISS National Lab look for ways to protect astronauts from its effects. Because many of the cardiovascular changes seen in astronauts resemble those caused by the aging process, such research also helps us in the search for ways to prevent and treat aging and heart disease on Earth.
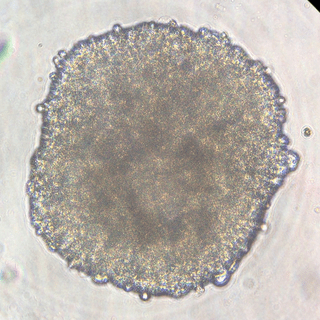
Many recent studies on the space station use tissue chips, small devices that mimic functions of human organs. These tools include three-dimensional (3D) cultures of specific types of cells, tissues made from cells engineered to reproduce specific characteristics, and even organoids or 3D structures made up of all the different types of cells in a particular organ, including the heart. These stand-ins for actual hearts enable new types of research and drug testing.
An investigation completed in 2018, Cardiac Myocytes, first showed that microgravity helps specially programmed stem cells move toward becoming new heart muscle cells. The experiment delivered frozen stem cells to the space station where crew members thawed and cultured them before returning the samples to Earth for analysis and comparison with control batches.
Subsequent research took advantage of microgravity’s effect on cell behavior and growth to create tools for further research, model disease, and test potential treatments for heart damage. MVP Cell-03 examined the production of heart cells from human-induced pluripotent stem cells (hiPSCs) in microgravity. Pluripotent cells are cells that have started to differentiate, making them more specialized than a stem cell, but that retain the ability to become multiple cell types. MVP Cell-03 showed that microgravity increased production of cardiomyocytes from hiPSCs. This increased production could make it possible to use cultured cells to help treat spaceflight-induced cardiac abnormalities and to replenish heart cells damaged or lost due to disease on Earth. Damaged human cardiac tissues cannot repair themselves, and loss of heart cells contributes to eventual heart failure.
“If we want to use these cells for clinical applications, we need to be able to generate a lot of them in an efficient way,” said MVP Cell-03 Principal Investigator Chunhui Xu of the Emory University School of Medicine and Children’s Healthcare of Atlanta. “Heart replacement therapy, for example, requires at least a billion cardiomyocytes for just one patient.”
The research also showed that space-grown cells have appropriate structure and function. That means they can be used to test drug safety. “Now we can test in a dish whether a drug causes adverse effects,” said Xu. This research can even use a person’s own blood cells to produce hiPCS cells and, in turn, heart cells that can be used to determine how the individual might react to a specific drug.
The next step is to look at the quality of cells produced with the Project EAGLE study, scheduled to launch later this year.
“In addition to making more cells, the other challenge is making good quality cells,” said Xu. “What we have in our dish now is immature cells. They don’t behave the way real heart cells behave but are more similar to embryonic heart cells. Transplanting those could be an increased risk for the patient.” Project Eagle looks at whether microgravity might be an effective approach to push the cells to more mature stages.
Xu’s lab also tested using cryopreservation, a process of storing cells at -80°C (-112°F), as an alternative to delivering live cell cultures to the space station. The team determined that cryopreservation does not appear to negatively affect the cells and even protects them from the effects of excess gravity experienced during launch. This technique makes it easier to plan future research since experiments do not have to start as soon as the cells reach the station.
For two other heart-related investigations, the ISS National Lab collaborated with the National Institutes of Health. Cardinal Heart, a study on the space station in 2021, used engineered heart tissues to confirm that microgravity exposure causes significant changes in heart cell function and gene expression that could lead to damage. Cardinal Heart 2.0, scheduled to launch to the space station in March, takes this research to the next step. It uses a beating heart organoid that contains stem cell-derived cardiomyocytes (beating muscle cells), endothelial cells (the lining of the heart), and cardiac fibroblasts (which form supportive connective tissue) to test whether certain drugs can reduce or prevent microgravity-induced changes. Using tissue chips to test new drugs could help reduce the need for the animal studies required before clinical trials in humans, potentially shortening the time between discovery of a drug candidate and its clinical use.
Engineered Heart Tissues, a BioServe payload launched to station in 2019, detected changes at the cellular and tissue level that could provide early indication of cardiac disease. Engineered Heart Tissues-2, scheduled to launch later this year, uses 3D cultures of cardiac muscle tissue to test therapies that may prevent these changes.
Studying the heart on the space station has yielded significant progress toward improving the health of astronauts and people on Earth. And that is worth celebrating, this February and beyond.
Melissa Gaskill
International Space Station Program Research Office
Johnson Space Center