“Houston We Have a Podcast” is the official podcast of the NASA Johnson Space Center, the home of human spaceflight, stationed in Houston, Texas. We bring space right to you! On this podcast, you’ll learn from some of the brightest minds of America’s space agency as they discuss topics in engineering, science, technology and more. You’ll hear firsthand from astronauts what it’s like to launch atop a rocket, live in space and re-enter the Earth’s atmosphere. And you’ll listen in to the more human side of space as our guests tell stories of behind-the-scenes moments never heard before.
Dr. Brian Crucian, a biological studies and immunology expert, discusses the hazard of hostile and closed environments in space for episode 61. Crucian serves as the principal investigator for a NASA functional immune study. This is part five the five-part series on the hazards of human spaceflight. This episode was recorded on June 28, 2018.
Exploration to the Moon and Mars will expose astronauts to five known hazards of spaceflight, including hostile and closed environments. To learn more, and find out what NASA’s Human Research Program is doing to protect humans in space, check out the “Hazards of Human Spaceflight” website.

Transcript
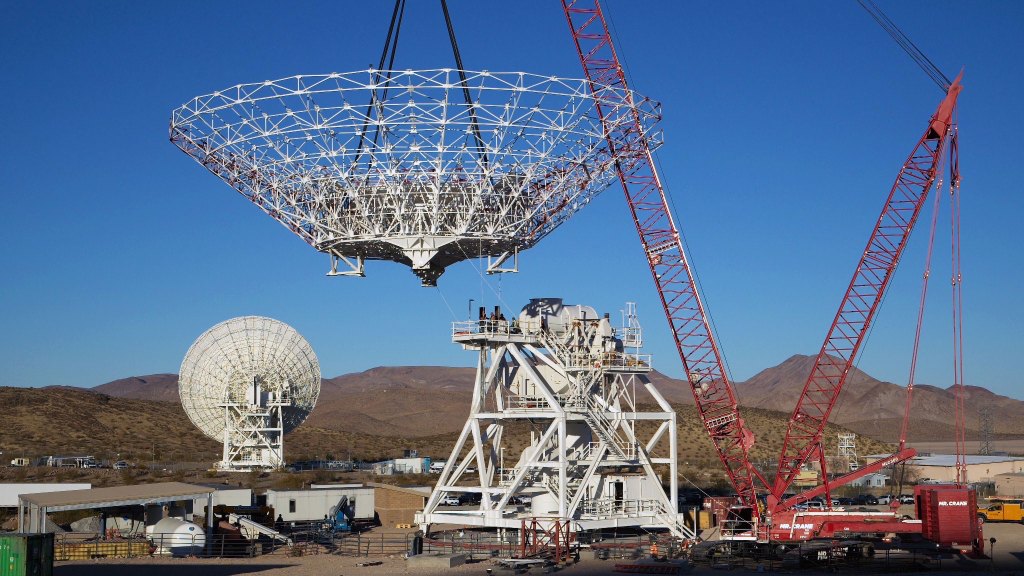
Gary Jordan (Host): Houston, we have a podcast. Welcome to the official podcast of the NASA Johnson Space Center, episode 61, Hostile and Closed Environments. This is part five of our five-part series on the five hazards of human space flight. How many times can I say five in a row? Five times. I’m Gary Jordan, and I’ll be your host today. On this podcast, we bring in the experts, NASA scientists, engineers and astronauts, all to let you know the coolest information about what’s going on right here at NASA. So, today, like I said, is the final chapter in this five-part series. The Human Journey to Mars is an extremely complex undertaking and challenging hazards such as radiation, isolation confinement, distance from Earth, gravity, and this last one, hostile enclosed environments are being studied using ground-based analogs, laboratories, and of course the International Space Station, right above us. Today we consider closed and hostile environments with Dr. Brian Crucian, a biological studies and immunology expert at the Johnson Space Center. Brian serves as the principal investigator for a NASA functional immune study. According to him, “the immune system is very complex, and several aspects of immunity remain uninvestigated during space flight.
We now need to delve deeper into the immune system changes that happen in space and determine if these changes during flight elevate clinical risks for astronauts in future deep space missions.” We’ll also hear clips from my conversation with Dr. Stan Love, NASA astronaut and just a super smart guy. Love shared his own perspective about living in a hostile and closed environment himself, and some thoughts about what it will take to make a successful deep space mission. So with no further delay, let’s go light speed and jump right ahead to our talk with Dr. Brian Crucian. Enjoy.
[ Music ]
Host: Brian, thank you for coming on the podcast today.
Dr. Brian Crucian: It’s a pleasure.
Host:So, this is last in our series of five hazards. We’ve talked to a lot of experts on the different hazards of space flights, particularly dealing with the human body, but this last one I think might be one of the more interesting, at least to me, is hostile and closed environments, because how I think of it is, you know, you kind of have to almost invent your own planet or earth, something that’s going to contain the human body in a livable space in the not so livable, you know, interplanetary space, and then carry it from one body to another. It’s such an interesting concept. But you’re an expert in immunology, so I think we should kind of start there, is when we’re talking about a hostile or closed environment, where does immunology come in?
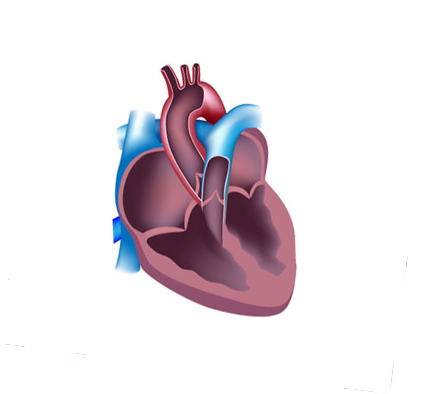
Dr. Brian Crucian:Humans need a well-functioning immune system to maintain our health, and that means protecting us from pathogens, viruses, bacteria. On the way home, someone may sneeze on you, and you might catch a rhinovirus or an adenovirus, and you’ll have a cold, and you’ll be sick for seven days. And so you need a well-functioning immune system, all these different cells that are in the blood and the lymph nodes to keep you healthy. But you also need a well-maintained, a well-tuned immune system, and so the immune system can go out whack. And if it is hyperactive, you might be at risk for things like allergy, asthma. If it really persists as a problem, you might develop autoimmune diseases. You also need a healthy immune system to keep you from getting other diseases such as cancer. One of the functions of the immune system is to keep you from getting cancer. We have cells in our body called natural killer cells, and they scavenge the body for malignant cells and eliminate them. And so you need a very well-maintained and properly operating immune system, and when you go into an adverse environment, such as space flight, or there are terrestrial adverse environments, the immune system can become dysregulated, and we say dysregulated, not suppressed, because it can be functioning too little or functioning too much, a little hyperactive, and so we, at NASA we have a variety of assays that we can monitor the immune system of the astronauts and see how well their immune system is functioning during space flight.
Host:So what do we know right now? Let’s just, let’s go to the International Space Station. What’s happening to the immune system up there right now.
Dr. Brian Crucian:Well, if you don’t mind, I’ll back up a little bit before that.
Host:Oh, please.
Dr. Brian Crucian:And so, as immunologists, our community, and this is immunologists in Europe, Canada, Japan, Russia. Our community has been very interested in what happens to people during space flight because we all want to get ready for those exploration missions, those deep space missions. And so when we head the space shuttle, all right, you could get a sample, a blood sample or a saliva sample from someone, look at their immune system after space flight. And if you get a sample from someone after space flight, what you’re really looking at are the stresses of landing. Landing is scary. Re-adaptation after a prolonged deconditioning is a stressor, and so you’re really looking at those stressors. And so we needed the International Space Station to come along to give us two things. We need long duration space flight, all right, because if you look at people during short duration space flight, you’re looking at the sprint. We want to look at the marathon because that’s more like a Mars mission or a prolonged lunar mission, right. And we also need the ability to sample them and return those samples during that long duration space flight. And so we needed the advent of this national laboratory to afford us the ability to look at what happens to people during long duration orbital flight.
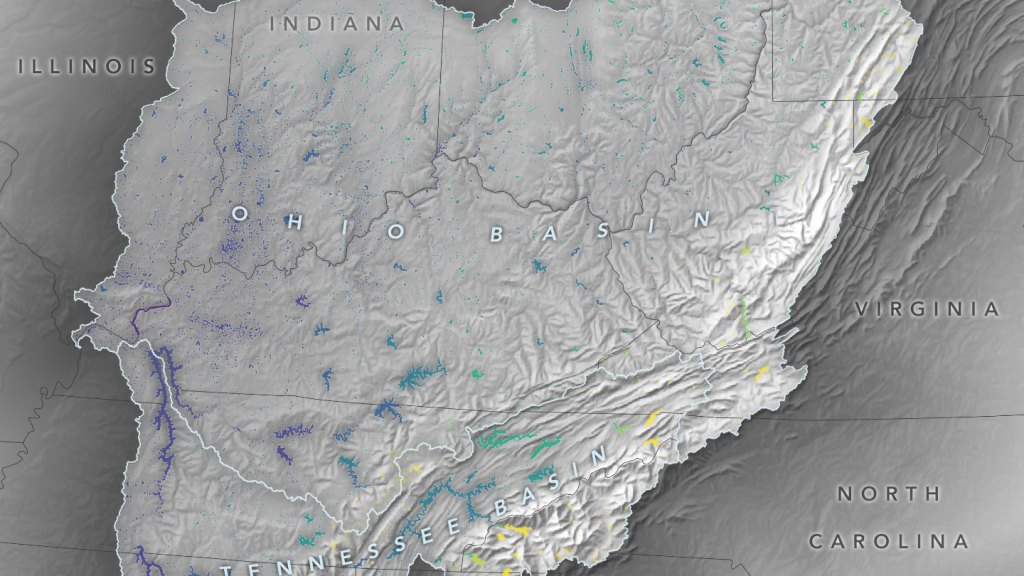
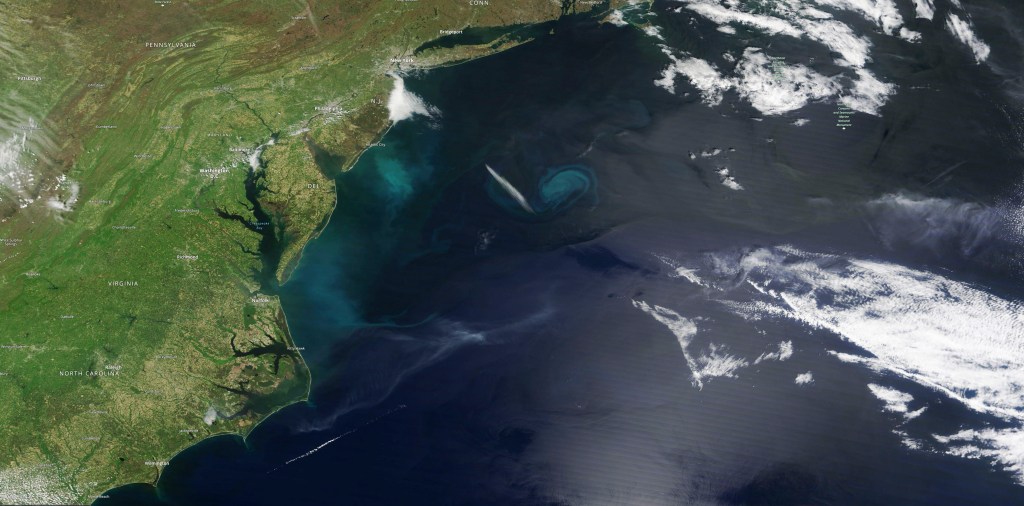
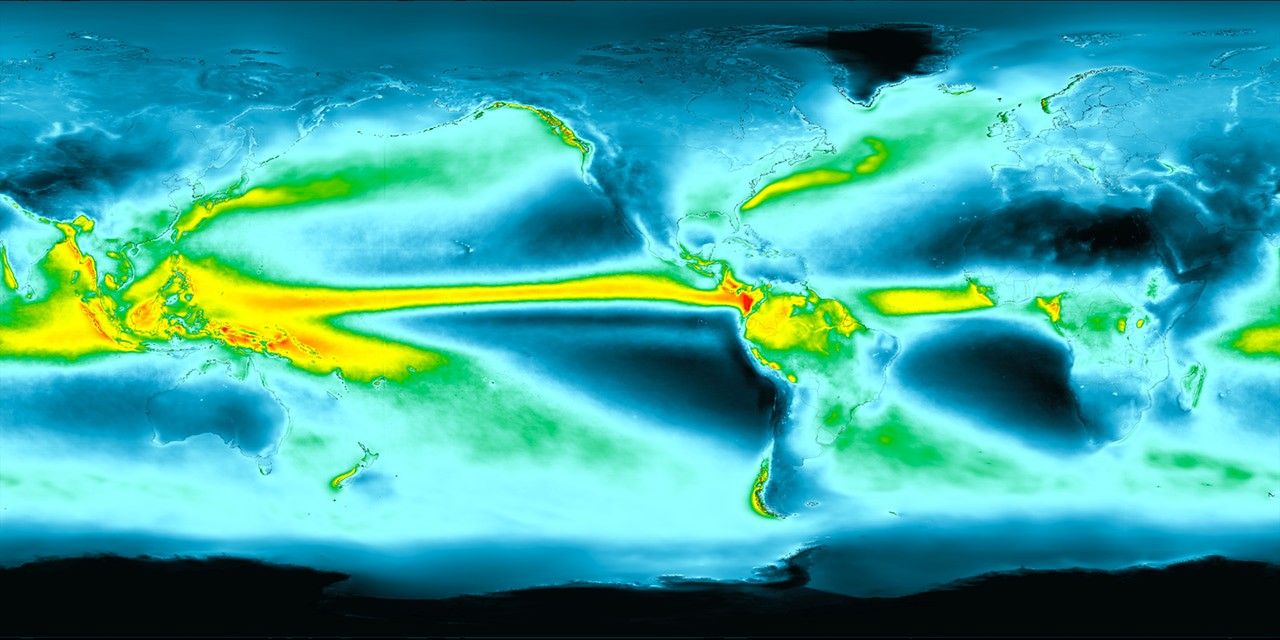
And in this situation, we’re using orbital space flight as an analog or model for those exploration missions. We have other analogs or models we use on Earth as representative space flight, for example, Antarctic winter over or undersea missions.
Host:Okay. All right. Do they all give us different and relevant data points that help us understand deep space flight, then?
Dr. Brian Crucian:Yes, we are learning through a variety of flight studies that have been happening on board the International Space Station. We’re learning what happens to the immune system during long duration space flight, all right, and there is an early adaptation phase, which is say the first 45 days where you’re adjusting to the environment and getting used to those new stressors, this hostile environment, and then you settle out into what we call space normal. And so we’re really more interested in sampling people on say the back half of their six-month mission so we can see what their immune system and other physiological systems also, what they have settled out to be for space normal. We think that’s more reflective of what might be happening during say a mission that would take several years to Mars. This will allow us to think about countermeasures for this phenomenon. Design those countermeasures while we have ISS, maybe validate those countermeasures so we can keep astronauts safe during those deep space exploration missions.
Host:So what do we know about the state of the astronauts at the end of their six-month increments. What state is the immune system in?
Dr. Brian Crucian:So the immune system is very complicated. It’s one of the most complicated systems in the body. You have many different types of cells. Lymphocytes, granulocytes, monocytes, and they all have distinct function. Some of these are comprised of what we call innate immunity that functions immediately. If you say puncture your skin, those cells go to work immediately, and they’re nonspecific. They want to eat those bacteria and heal that wound and protect you. You also have other types of cells that are what we call pathogen specific. If you get that virus on the way home, you get that adenovirus or that rhinovirus, you need virus-specific immunity. And so that takes about a week to generate and eliminate that pathogen, but that stays with you for the rest of your life, and you have memory to that particular virus. You never get the same cold virus twice. And so when we look at astronauts during space flight, we have to look at all these different aspects of their immune system to answer that simple question. What’s happening to innate immunity. What’s happening to adaptive immunity. The B cells make antibodies.
The T cells control viruses. The natural killer cells help keep us from getting cancer, and so it’s a complicated question, and we’re still looking at some of these aspects. What we have looked at very well have been molecules called cytokines in the blood plasma of astronauts, the molecules that regulate immunity, and we can look at them over the course of a mission and see what type of dysregulation, what type of inflammation we have. We’ve looked at certain types of cells, cells that control latent herpes virus reactivation, and we see those don’t work as well. That leads to the reactivation of certain types of viruses in astronauts. And so we’re characterizing this phenomenon in astronauts. They’re not sick at all. I mean they’re working hard and enjoying their missions, but these are subclinical phenomenon that make us a little bit worried about what might happen on a Mars mission that would take several years where you’re going to increase the radiation, and you have no rapid return option.
[sound effect]
Host:So next I ask about things growing on the space station, but before we get into that, Stan Love gave his own insight into things growing in the space environment and how that relates to planetary protection.
[sound effect]
Stan Love: So the microbes that are in your environment are the ones that you bring with you largely. Microbes have a very fast turnover rate, so they could evolve a little bit, change a little bit while you’re in space, but not a lot. I think they have isolated new microbes on the space station. The space station has been up there for ten years, so it’s had time. But planetary protection is actually something we need to pay pretty close attention to. The moon is probably as dead as a doornail. It has had no atmosphere for four and a half billion years. It gets irradiated by the sun, the ultraviolet light, the solar wind, the cosmic rays. There’s no water. The temperatures in the daytime are over-boiling. The temperatures are night are 200 degrees below zero, and we’re pretty sure, and we’ve got the samples back from [inaudible], of course, and we’ve looked through them, and we have found nothing alive. We did find some spores on a TV camera, on a probe we sent to the moon, and then later the astronauts landed next to that probe and brought home the TV camera lens to study how it had changed in ten years, and they found some viable microbe spores that had not yet been killed, but those guys were not growing and multiplying.
Yeah, microbes are tough.
Host: Wow.
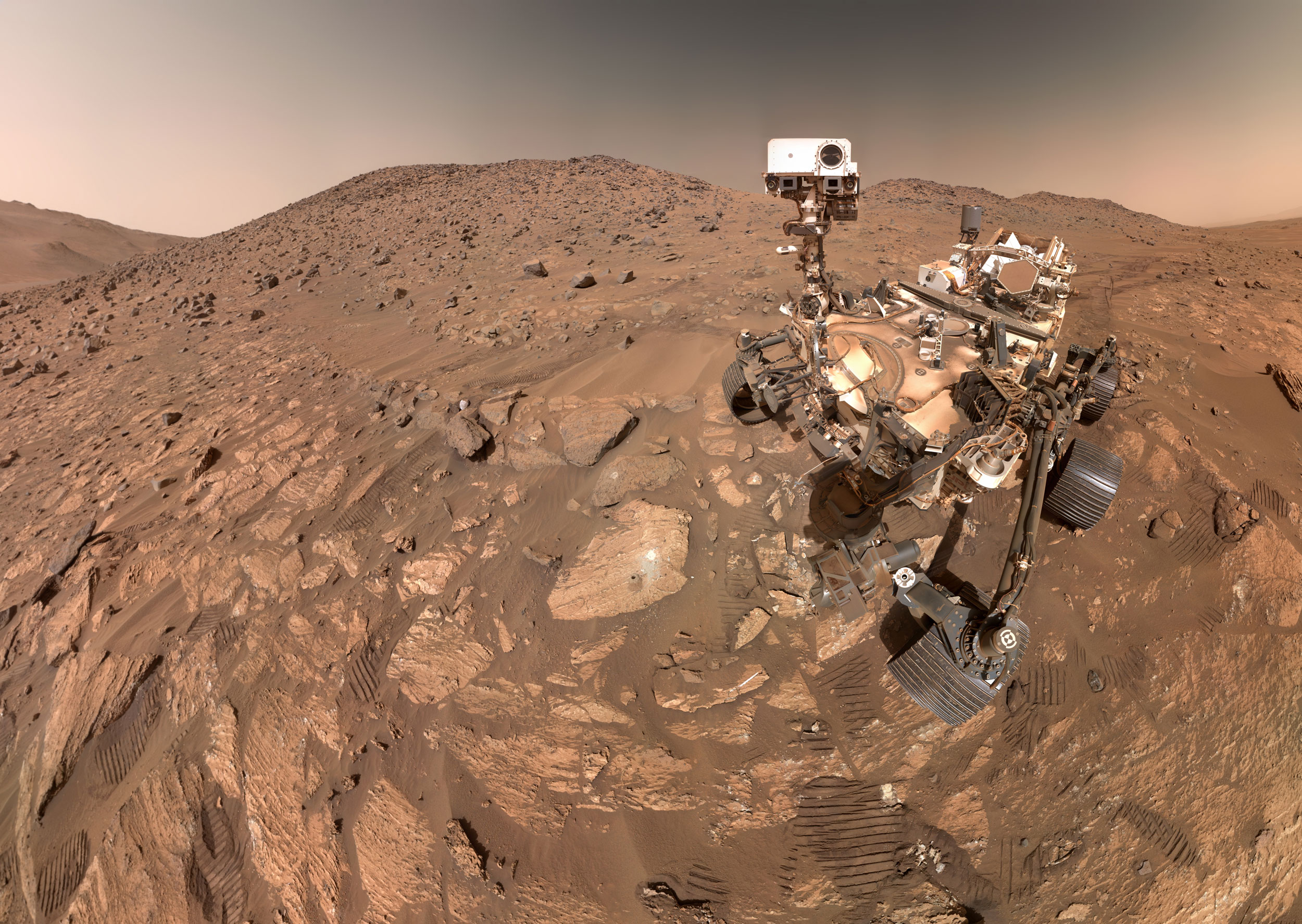
Stan Love: So with that in mind, microbes are very tough, when we talk about Mars, now that’s got an atmosphere. The daytime highs are not as hot. The nights are cold, but the nights are cold in Antarctica, and there are algae living inside rocks in Antarctica that can only photosynthesize during the summer when the sun comes out. So life is pretty tough, and there might be microbes on Mars that when they got into a nice, warm, moist, happy Earth environment would go berserk and destroy our lives here.
Host:That would stink.
Stan Love: Okay, the odds are low, but the risk is terrible. Have you ever seen the movie, The Andromeda Strain, it gives you a hint of what could possibly happen. That one came back from Venus, and I’m not worried about Venus. Venus is probably really sterile.
Host:It’s pretty hot there.
Stan Love: It’s really dang hot, yeah.
[sound effect]
Host:Yeah. Would then, it would be something that would develop internally or would it be something maybe from the environment. Because just from having conversations with some of the experts in the past, it seems like there’s, you know, fungus and just stuff growing in the space station. Is that something that’s a concern from an immunology perspective?
Dr. Brian Crucian:So that’s a great question, and what you’re basically asking is what causes it.
Host:Yeah, yeah.
Dr. Brian Crucian:And so that’s a complicated answer as well.
Host:Hum.
Dr. Brian Crucian:You have humans in space is what we called an applied experiment, meaning if I’m doing an experiment in my laboratory, I’m controlling one variable. I want to see if a certain diet or radiation or microgravity causes an effect. When I put humans in space, they’re subjected to a whole bunch of variables, and I can’t stop that from happening. So they’re experiencing stress, microgravity, radiation, alter circadian rhythms. They see a sun rise and a sun set every 90 minutes. Isolation and a confinement. And so what we’re really talking about is not the effect of microgravity but the effect of space flight on these people. And space flight is defined as all these variables. So all of these variables create a synergy, and they affect the human body adversely, and we see effects on bone, muscle, fluid shifts, the immune system, and so collectively, we at JSC and around the world, these scientists are trying to characterize these phenomenon so we can develop counter measures.
Host:Hum. So what do we know about counter measures that we, do we have counter measures right now? What are we doing to, based on what we know and recognize, are there things that we have in place that can sort of help protect the immune system on board.
Dr. Brian Crucian:Well, that’s another big question. We can probably spend an hour talking about counter measures–
Host:Hey, we have an hour.
Dr. Brian Crucian:And I’ll try and keep it to the 50,000 foot level. And so, yes, we have counter measures that are already in place. Things that you might not consider a counter measure are in fact a counter measure. Radiation shielding is a counter measure. Maintaining a clean spacecraft is a counter measure. Propulsion is actually a type of counter measure. If you can get me to Mars in two weeks, a lot of the problems I’m worried about go away.
Host:Oh, yeah.
Dr. Brian Crucian:But what people classically think about is say the pill that you would take as your counter measure.
Host:Right.
Dr. Brian Crucian:And so we, for the immune system, we would look at things like nutrition supplements, probiotics, things that you can take to reduce inflammation and actually medications, pharmacological interventions can influence the immune system. And so where we stand in my discipline is we’re trying to characterize this phenomenon, and we’ll defer our selection of countermeasures until we’ve completed characterization, and there are several European, Russian, and American studies that are working to characterize this phenomenon. Then we’ll sit down with researchers, flight surgeons, practicing clinical immunologists and collectively look at this data and then try and figure out, okay, what will the counter measure be for the immune system. Other disciplines I’m sure have the same discussion with their experts. When you’ve selected your counter measure, then you would probably want to look at that in the ground environment first and validate it, and if there’s time, within the life span of ISS, you would want to do an in-flight validation also.
Host:So we have a lot of data on the International Space Station already. You know, we’ve been up there for nearly 18 years at this point for continuous human presence, just a lot of people going up and living there, successfully too. We do things, like you’re saying, with counter measures, just wiping down the inside of the space station. So what do we understand about living in a closed environment so far? Do we even have to worry about some sort of external, I mean I’m thinking, when I think of immunology, the first thing I think about, like you’re saying, is like a common cold. There’s just some sort of virus bacteria, something that can affect, you know, I guess us in every day life, but an astronaut, you know, do we even have to worry about that in a closed environment?
Dr. Brian Crucian:Well, the answer is yes, and we learned that early on in the space program. If you’ve ever seen the great movie Apollo 13, you know about how a space mission can be affected by clinical disease, either before the mission or during the mission, and in fact, we had several infectious disease events during the Apollo program, and that led to the implementation of the health stabilization program, which is basically your preflight quarantine. After that was implemented, the rates for infectious disease during space missions went down. And so that was one of the first operational countermeasures that was really put in place to help keep astronauts healthy during their space missions. There are other types of operational countermeasures that we’re doing today. We screen, you seem to be asking about environmental concerns, and we screen food that goes up, payloads that go up. Get a toxicological screen, a microbial screen, and so we’re trying our best to keep this environment clean and that will help keep the astronauts safe.
Host:Yeah.
Dr. Brian Crucian:And as we continue to characterize things that happen to physiology during missions on ISS, you’ll start to see more discussion of these biomedical counter measures, just something that someone might ingest to supplement or a medication. But collectively, all of these operational counter measures and counter measures that are ingestible, will be employed on these deep space exploration missions.
Host:For sure.
Dr. Brian Crucian:The cleanest environment, the fastest space ship, the most pristine foods and water that we can get, and this wonderful set of medications to help keep people healthy.
Host:Man, that sounds like a great place to spend some time in space. Yeah, that’s a good vehicle, the one you’re describing.
Dr. Brian Crucian:You can set it up. I’m willing to go with you. [laughter]
[sound effect]
Host:So that’s a great overview of what we know so far about living on the ISS. Stan Love added a few more details outside of immunology, and there’s a lot here, about ten minutes worth of stuff, but stick with me, because it’s super interesting and totally worth it. And we’ll get back into the immune system afterwards.
[sound effect]
Host: Now how about the International Space Station specifically. What are we learning, what are we learning on there about living in a closed environment, maybe about lights, maybe about air, maybe about stuff like that?
Stan Love: Well first of all, with the confinement of small volume, space station crews to my knowledge have never complained that there wasn’t enough room. So the space station is good for at least six months, but the space station is really big, and we can’t sent it to Mars because it’s too big.
Host:Yeah.
Stan Love: Lighting, lighting on the space station early on tended to be kind of dim, and there was enough light for people to do their work, but it affects your mood, your emotional state, if the lights are too dim all the time. Getting exposure to sunlight is important for keeping your biological clock running properly, so you feel sleepy at bedtime, you sleep well at night, and then you wake up refreshed in the morning. That’s not a given in space. We’re going to Mars without planet to interpose itself between us and the sun to make night. It’s always going to be full sunlight outside, but there aren’t going to be very many windows, so it’s going to be artificial lighting inside. Lighting on the space station has been gradually changing out with brighter lights and lights that you can change to be blueish in the morning, and that helps your biological clock to say, oh, it’s morning. It time to get up and be energetic, and they can actually make them a little bit redder in the evening on the space station. And that tells your biological clock, oh, the sun is going down. I should be getting ready to have a meal and go to sleep.
So we’ve got that capability on the space station now, and I haven’t heard anybody complaining about the light. So I think we’ve got that. Food, water, and air are crucial. We don’t last long without those, and for Mars, we cannot take enough fresh water in tanks to keep the crew hydrated for six months, nine months out, a year on the surface of Mars, nine months back. So we’re going to have to recycle our water. And yes, that’s gross. And my buddy Spanky, who’s spent a couple of tours on the space station calls it turning yesterday’s coffee into tomorrow’s coffee.
Host:I love that.
Stan Love: So that piece of equipment, first it has to work really well. If your water starts tasting like pee, you’re going to be an unhappy person.
Host:Oh yeah.
Stan Love: And eventually an unhealthy person. And if it breaks, you’re stuffed, right.
Host:Oh, yeah.
Stan Love: You are in terrible trouble, and unfortunately this kind of closed life support, you know, where we recycle most of our water, so we can distill clear water out of urine, the stuff left behind is so gross you don’t even want to think about it. It’s like dark brown, ammonia, stinking sludge.
Host:Oh, now I’m thinking about it.
Stan Love: Yeah, oh, so, okay. So that part we can’t recycle, although we’re thinking about ways to get even, squeeze even more water out of that, but I hope that works really well because the sludge that it’s coming from is not appetizing. You have to do the same thing with your air. You inhale, actually most of our air is nitrogen that our bodies don’t use. But you inhale, you burn up some of that oxygen, you exhale some carbon dioxide. You’ve got to pull that carbon dioxide out of the atmosphere. Over the years, that’s given us a lot of trouble. We had what we thought were machines that could keep the carbon dioxide in the atmosphere down to a nice low comfortable level, but we’re finding out that with six months of exposure, a level of CO2 that you wouldn’t even notice, CO2 carbon dioxide, that you wouldn’t even notice if you were exposed to it for a day, if you were exposed to it days on end, it starts giving you headaches. There are mood changes. People get irritable. It adjusts the chemistry of your blood if you’re breathing a lot of carbon dioxide. That’s what actually triggers your breathing reflex, those changes in the acidity of your blood.
Host:Ooh.
Stan Love: Good stuff. And so we’re finding that for a long duration, we need to keep the carbon dioxide down at a low, low level where our machines can barely keep the CO2 down there, because you’re trying to scrub, you know, if scrubbing carbon dioxide out of air was easy, we wouldn’t have any worries about climate change. Getting carbon dioxide out of air is hard. It takes a lot of power, complicated machinery, things that absorb carbon dioxide when they’re cold, and then you seal those off, open a vent to the outside, heat it up, and drive the CO2 out overboard. Where now we actually can take the carbon dioxide and water that people are exhaling, you also exhale water vapor that has to be captured from the cabin atmosphere and removed or the humidity gets really high and it gets real sticky and gross inside. So all that stuff has to work, and we have to try to recycle some of it, and we can actually convert some of that captured oxygen and carbon dioxide back to water and oxygen that we can use.
Host:Nice.
Stan Love: So that part is good, but then we’re dumping methane overboard. Well we could keep that methane and use it for rocket propellant, if we were very clever about it. But there’s going to be some loss, but we have to recycle and recycle and recycle because we just can’t carry all that much raw materials. And so that equipment becomes crucial. If it breaks, you’re going to die. They gloss over this quickly in the Martian if you saw that movie or read the book.
Host:Yeah.
Stan Love: The science is even better in the book. The movie did a pretty good job. The book does an excellent job. He sort of glosses over, yeah, the air recycler has to keep working, and it never broke, so that was good, because he lived.
Host:Right.
Stan Love: And when you think about space ships, you know, we have satellites that do communications, that take pictures of the Earth. We have robots that go out to the planets, and we’ve launched thousands and thousands of these things over the history of space programs. And all of them have a power system and a computer system and a communication system and structures and thermal control and all these other systems, only a couple have had life support systems. So we have millions of hours of run time on basic spacecraft mechanical systems. We don’t have as many hours on life support systems. So this technology is in its infancy compared to most of the things that are on space ships, and hence, they break a lot. You know, on the space station that’s fine. We have a lot of spare parts on the space station and we can send up more with, you know, six weeks of notice, because we got robot ships going up there all the time.
Host:Yeah.
Stan Love: On the way to Mars though, nah ah. You don’t have a possibility of resupply. You can prestage some stuff at Mars, but as we like to darkly, humorously point out, if your life support system breaks halfway to Mars, you have the rest of your life to fix it. [laughter]
Host:That is pretty dark but pretty funny.
Stan Love: Yeah, so, but it gets the point across, right.
Host:It does, it does.
Stan Love: You’ve got to get this repaired or you’re going to die.
Host:Yeah.
Stan Love: And it must recycle because we cannot bring raw materials. The one things we can’t recycle yet at all is food. So turn poop into a salad, only the Earth can do that for you.
Host:Ah.
Stan Love: Okay. Only the Earth can turn your poop into salad.
Host:Right.
Stan Love: And I mean an appetizing salad. So we, a farm needs sunlight. Sunlight is something like 1000 watts on every square root yard of plants.
Host:Wow.
Stan Love: And when you figure out how much grow lights that is, no space craft power system can support that. Even if you made a farm and grew a couple of very selective crops on small areas that was barely enough to feed the crew, plants get sick. Single species plants get sick easy. And if a, you know, rust wipes out your wheat crop halfway to Mars, you’re out of luck, right. You got no harvest, you’re dead.
Host:Yeah.
Stan Love: And, you know, this was a problem for humans in antiquity. We’ve gotten better at that, you know, with fertilizers and, you know, pest treatments for our crops, but it’s tough to re-create a farm in a space craft. The power, the weight, you could use sunlight, but now you need giant windows, engineers hate little tiny windows because keeping the air pressure inside from blowing the window out to the outside means heavy structures and triple panes of glass, and that gets big and heavy and you can’t make a greenhouse. The same thing on Mars. It doesn’t have enough air pressure to hold your greenhouse down, the internal pressure from normal air is 15 pounds on every square inch of that glass on the greenhouse. So farms are a long time coming.
Host:Yeah.
Stan Love: People who study this problem professionally gain a new appreciation for the services that we get from the Earth without paying for them. These would be very, very expensive if we had to try to reproduce them from scratch. There was even a long-term experiment that was built and run in Arizona called Biosphere 2, and they built this gigantic greenhouse, and they seeded it with miniature biomes, like a jungle and a coral reef and an ocean and tried to re-create a miniature Earth’s environment, totally sealed from the outside, and they put six people in it, and they were going to try to live there for a year or so. And the results were not good.
Host:Really?
Stan Love: Okay. The bees that they had for pollinating all died immediately. The ants and cockroaches population exploded. The oxygen in the atmosphere began disappearing. They had to pump in extra oxygen.
Host:Oh wow.
Stan Love: To keep the crew from perishing.
Host:Right.
Stan Love: Strange, horrible chemicals started showing up in the environment that were eventually traced to the body fat of the crew members, you know, from eating, you know, apples that had some pesticides or something on it. They had this in their body fat, and they lost so much weight that those chemicals were showing up in the environment.
Host:Wow.
Stan Love: And eventually they had to terminate the experiment, and there were many, many things that were problems with that, not just the technical, the management was difficult as well. But look it up sometime and think about, okay I have to make a new biosphere too, and if any part of it fails I’m dead. And, you know–
Host:It gives you a lot of appreciation for the Earth.
Stan Love: Yes.
Host:Because the Earth does a pretty good job of keeping us alive.
Stan Love: Earth does an awesome job, and we should not mess with that capability because we are highly invested in it, I like to put it, we are highly invested in the status quo.
Host:Oh yeah.
Stan Love: So, farms and space are going to be a long time coming. Appreciate what you got here.
[sound effect]
Host:So that’s the environment, and it seems, it seems pretty straightforward, right. You want a clean space craft, you want a fast space craft, you want one with enough food. Now what are we doing to make sure that the astronaut’s immune system is strong? Are there stuff, is there like exercises or something, maybe, I don’t know, getting enough sleep is something that really helps with keeping the immune system strong in space.
Dr. Brian Crucian:Well, what you’re really getting into are translational aspects of physiology that can influence the immune system. And so exercise is important to keep the immune system strong. If you don’t exercise, you will become somewhat immune deficient, and you should exercise to maintain your immune health and other aspects of your body. Too much exercise though, can have an adverse effect on the immune system. Marathon runners have a higher incidence of infectious diseases after completing these races, because it’s a stressor on the body. It’s like most things in life, there is a sweet spot of activity where you want to be not too much and not too little.
Host:That’s right. That’s why I don’t run marathons really. I just don’t want to get sick.
Dr. Brian Crucian:I’ve done three. It’s very challenging. I’m a middle to the end of the pack kind of guy.
Host:Did you get sick afterwards?
Dr. Brian Crucian:No.
Host:Oh, okay.
Dr. Brian Crucian:But I wouldn’t say that I was really physically exerting that much. [laughter]
Host:Middle to the, oh, I see, I see, yeah. So was that, is that really a consideration for space flight then, making sure that even if they are exercising, because it does help with the immune system and sleeping enough, that they’re not doing so, they’re not exerting themselves too much. Is that a consideration for maintaining immune health?
Dr. Brian Crucian:That’s an interesting question. And NASA and our wonderful exercise experts here have been working this for decades. Different types of aerobic and resistive exercise devices have been employed on ISS, and we’ve been looking at their effects on bone loss, muscle loss, and it’s getting better is my understanding. This is not my area of expertise, but certainly all of these exercise counter measures are having a positive effect. Some crews don’t lose that much bone and muscle as compared to early in the space program.
Host:So on top of exercise, you know, we’re talking, we’re talking sleeping too. You know, we actually had a conversation, I think it was, oh, gosh, we’ve had a lot at this point. I want to say it was with Tom Williams, we talked a little bit about sleep because he did a number of sleep studies, but how sleeping is, I guess, affected to the immune system, and you mentioned a little bit about circadian rhythm too, seeing 16 sunrises and sunsets per day.
Dr. Brian Crucian:Right. Proper sleep, enough sleep is also very important for maintaining a healthy immune system, and you have a circadian rhythm that helps you sleep well at night, and so cortisol is a stress hormone, levels of cortisol will fluctuate throughout the day. Your peak cortisol in your blood or saliva is about 30 minutes after waking. You’re up and ready to go. It tends to trail down for the rest of the day, get you ready. Your lowest levels are at night before sleep, get you ready for sleep, and so a proper immune system also requires sufficient sleep and also requires a well-maintained circadian rhythm. What happens in space is they rapidly lose their circadian entrainment, and what we see is sleep medications are probably the most commonly used medication on orbit.
Host:Really?
Dr. Brian Crucian:To help the crews get a proper night sleep. And so one of the things that is probably contributing to the dysregulation of the immune system we see on orbit is definitely a loss of circadian entrainment in these crews. We can look at the effects of sleep loss terrestrially, either in a laboratory setting, Steven Chia [phonetic] did a nice study where he looked at the immune system of people that either didn’t get enough sleep or that were shifted, one or two hours a day, over the course of a week, to look at just the effect of sleep on the immune system. We can also look at people doing a winter over in Antarctica. And so crews spend a year in Antarctica, they spend several months in a period of 24-hour darkness, and so that has a profound effect on their physiology, and we are, along with European collaborators, in particular Dr. Alexander Chokair [phonetic], we are looking at what happens to the immune system in several Antarctic bases. Antarctica is a mountain, and so some of the interior bases like South Pole Station or Concordia you get these sleep alterations, the circadian loss, this 24-hour darkness, and you also have a persistent hypobaric hypoxia, coastal Antarctic winter over.
You have a normoxic environment, but you also have that extreme environment. And so, yes, in-flight sleep is important. It can affect the immune system, and these are the tools we would use to look at this phenomenon on the ground.
Host:Hum, Antarctica, wow. I mean, if I was going to go to Antarctica, I’d probably choose a 24-hour light. That would probably make me feel a little bit better.
Dr. Brian Crucian:They have that during the Antarctic summer.
Host:Yeah.
Dr. Brian Crucian:And then when we get to the Antarctic winter, they get the 24-hour darkness.
Host:Right. I don’t know why you’d sign up for the Antarctic winter trip, but how long are they staying there to really get enough data to understand this circadian change?
Dr. Brian Crucian:Crews performing a winter over in Antarctica, at most of the bases, the typical mission duration is about a year. That makes it a fantastic ground-based space flight analog where we want a prolonged mission duration. So the year is dictated by the calendar year. Generally during the summer period in Antarctica, you have resupply of these bases. Crew swaps happen, and then the last crews leave for the winter over period, and the crews do their one-year duration with the middle of the Antarctic winter being the three months or so of 24-hour darkness.
Host:Hum. Do we have enough data to understand what’s happening to the immune system because of these sleep studies, or is there still a lot that we still need to look into?
Dr. Brian Crucian:Well, we have been, if you’re asking about Antarctica, yes, we’re learning more. People have been looking at the reactivation of latent herpes viruses, which is a nice biomarker for immune dysregulation in Antarctic winter over and during space flight for decades. Dr. Duane Pearson at NASA was one of the pioneers for using viral DNA in saliva as a biomarker for immune dysregulation. But more recently the studies I mentioned with our European collaborators are helping us to really define comprehensively what happens to the immune system during Antarctic winter over. And so a lot of the same assays that we use to characterize immune changes in astronauts that have happened on ISS, we simply translate those assays to Antarctica and employ them there, and it give us a very nice flight to ground comparison.
Host:Right.
Dr. Brian Crucian:What’s interesting is the different ways you have to change things to implement studies in these two different locations. And so for space flight, it’s very difficult to take our laboratory there or get a lot of crew time to do a lot of processing for the sample. So we’ll draw a blood sample. We’ll bring it back to Earth, and we can get an ambient blood sample in our hands in about 37 hours that was collected during space flight. For Antarctic winter over, you don’t have a rapid return for samples like this, and so you have to, you do have the ability to deploy a little more equipment. And so Concordia station in particular, we deployed flow cytometers, various sample processing apparatus, and we were able to have the crews do a little more remote processing of our samples during their winter over activities. But we’re chasing the same data. Flight to ground comparison is very important for validating a ground-based analog, which is a nice tool to help you understand what’s happening during flight and also a nice location then you can probably use to test your counter measures.
Host:Right. Yeah. There’s a lot of other, there’s a lot of other research going on too that’s– you used the word analog, that’s these sort of studies where you’re putting them in an environment that’s, you know, it’s not like you’re taking a vacation. I wouldn’t call that a vacation at all, but you’re really just putting them in this environment to really understand what it’s like in these hostile environments. Antarctica is one of them, and there’s another one called Mars 500 too. What’s happening there? Are we doing similar studies?
Dr. Brian Crucian:Mars 500 is a very interesting space flight analog that’s happening in Russia the Institute for Biomedical Problems in Moscow, and I should probably back up and give you the overview of these different types of analogs and how they work. And so analogs on the ground are wonderful for doing physiological assessments of people and learning a little bit about space flight without having to go there, but the choice of analog depends really on the system that you’re interested in. And so if I’m interested in bone and muscle loss, we use head down tilt bedrest. We put people in bed for 90 days, and they don’t move. Well, they move a little bit in the bed, but they don’t get up. They have this hypokinesis. They don’t use their bones and muscles as much. They are head down tilted, so you get fluid shifts as a great analog. It’s not a great analog for immune dysregulation because a lot of the stressors I mentioned before aren’t present in that analog.
Host:Right.
Dr. Brian Crucian:Antarctic winter over would not be a good analog for these bone and muscle scientists because even in Antarctica, you’re in a 1G field, and you’re carrying things around, and you’re ambulatory and you’re walking about. And so you have this whole suite of analogs that differ. We also have cell culture analogs and animal analogs, a whole host of tools we can use. Mars 500 is a really nice analog where they’ve re-created the interior of a space vehicle, and they put people in it for up to 500 days and simulate the entire anticipated duration of a Mars mission including landing day, and then they have them exit the vehicle and do a little simulated planetary exploration in space suits, reenter the vehicle, and so to pretty high fidelity, they re-create a Mars mission and except your lacking the radiation component, the microgravity component, but most other aspects of the flight can be replicated. They even did communication delays, I believe, to make it more realistic.
And we did have some of our European Russian collaborators do immune assessment on the Mars 500 participants and did see some interesting changes that some aspects of which did look like space flight. And so there’s probably a psychological stress component to what is happening to the immune system also.
Host:Right. But this is, this is an analog where you don’t have, you’re not able to play with microgravity because this is happening in Russia. So you’re taking away some of these components that really fully encapsulate what it’s like, the space flight environment basically, but you’re still getting immune responses just based on being in the environment, the stress of it. What is, what is, I guess this might be a fundamental question, but what is stressful about being in a closed environment for up to 500 days?
Dr. Brian Crucian:Well, you’re right in that we cannot in an analog replicate all the factors associated with space flight.
Host:Right, which is why [inaudible].
Dr. Brian Crucian:When I lecture students, I tell them two things in particular. We can’t really put people in a microgravity room. We don’t have something like that, and the boards that regulate our science frown on me irradiating people. So you’re never really going to get the radiation, the microgravity component, but as you said, there are a lot of other stressors that influence people during space flight. Those can be replicated to pretty high fidelity on the ground, the psychological aspects, the confinement, the circadian shifts, the stressors. One of the things we prefer for immunology are in fact, these aren’t really analog missions or mission simulations. If you go to Antarctica, that’s a real mission with real risk to self. It’s a dangerous place down there. The air craft operations down there and the extreme temperatures, and so we call them space flight analogs, but in fact these are real missions to dangerous places. So, to answer your question about what is stressful, there are different types of stress.
There are psychological stressors. There are physiological stressors. You being away from loved ones or being in a confined small craft is a psychological stressor. Circadian misalignment might be a physiological stressor. You have different mechanisms in the body, most of which are regulated by the immune system that control stress and your response to stress. You have something called the fight or flight response.
Host:Right.
Dr. Brian Crucian:Which is you’re either going to ramp up your adrenaline levels and want to engage that stressor if it’s an acute stress, or if it’s a chronic stress, you see changes mediated by the cortisol, which are generally immunosuppressive. Elevated levels of cortisol are really not good. And so space flight is a very unique stress model, we have learned through our data over the years. It is a six-month long chronic stressor with intermittent acute stressors. Space walks, stressful events on orbit. Sometimes we purposefully circadian shift the crews because a vehicle is going to dock or undock.
Host:Right.
Dr. Brian Crucian:And so we don’t really have a stress model like that on the ground, which is one of the reasons why the flight data that we’re seeing may be so unique. I think you asked about the flight-to-ground comparison, and yes, in some of these analogs from an immunological perspective, they look like flight, but we haven’t seen one yet that looks exactly like flight. And we look at dozens of different types of immune proteins in the blood, cytokines, and the distribution of these cells and their function. We look at immune cell function in cell culture assays that we do. And we haven’t seen anything yet that looks exactly like flight.
Host:Well, you need to put them in the room with a gravity switch and blast them with radiation, and there you go.
Dr. Brian Crucian:Well, the IRB frowns on us doing that, so until then, we’ll struggle using the closest analogs we can find and actually look at people during their missions, which is even better yet.
>>1Right. So we talked a little bit about, you know, when we’re talking about counter measures, just ways to prevent these, any sort of immune, I don’t know, sickness, any kind of sickness when it comes to these astronauts. There’s a lot of things that you don’t think of directly as counter measures, like, for example, getting a cold and taking cold medicine, but– well maybe that’s not a counter measure. It’s more of like a, I guess way to treat it. But, yeah, what are some curious ways that we are, I guess, reducing the stress for the astronauts on board, making, I guess, just a friendlier environment. It is a hostile environment, but as friendly as we can make it so that we’re reducing their stress.
Dr. Brian Crucian:Well, what you’re describing is a very bona fide approach to keeping astronauts healthy. We want to reduce their stress, and so we enable them to talk to their families. There’s actually a satellite phone on board the space station, and they can call home when they need to. We try and create work schedules that are palatable for them. We don’t want them to be working constantly and wearing themselves out. They’re working hard enough as it is, but we want to keep them healthy, and so we properly regulate their work schedules. They’re assigned psychological support folks on the ground that help get them say a TV show that they’re interested in for free time or something like that, and so psychological support is very definitely something that it’s happening on board ISS and something is being taken very seriously for the pending exploration missions.
Host:Right. So it’s these, these elements will be probably, I guess you can say they will be part of the exploration mission. So if you have a long duration stay to Mars, they’re going to be sending them these movies and just ways to sort of relax along the way, but then also there. They’re going to have to have some break time.
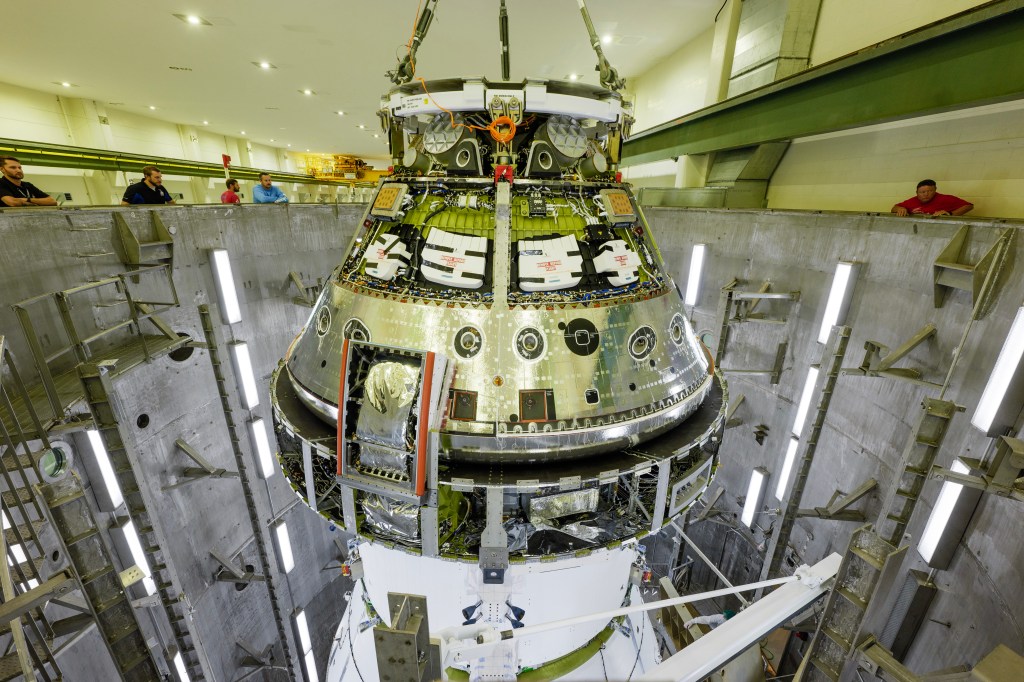
Dr. Brian Crucian:Yeah, what’s interesting about considering the lunar missions or Mars missions that should happen by the 2020’s, it’s nice to see all that moving forward, is the vehicle design is happening now. And so, on ISS, you’re not far from home, and you have a tremendous amount of space with which to start to deploy exercise equipment, sleep compartments, carry a log of food, and these pending, these upcoming exploration missions, the situation will almost be the opposite. You’re not going to have a return option. You’re going to have a very small vehicle, and so one of the challenges I think NASA and international partner space agencies are dealing with is how to maximize the reductions in stress and the crew comfort and crew health on these missions while doing it farther from home, in a higher energy radiation environment with more stress.
Host:Yeah, yeah. Now, thinking about missions, I guess beyond the space station, you know, now that we’re kind of going towards that topic. I’m thinking about systems really. I’m thinking about, we’re talking about a hostile environment, making the environment as I guess more comfortable, to make sure the crew is happy and healthy, which is very directly related to the immune system. Because the happier they are, the healthier they are, you know, psychologically, physiologically, they’re going to be successful on these missions. But the systems that they’re in, the closed environment that they have to be a part of, is a concern just in and of itself because right now on the space station let’s just say, you know, the toilet, they have to fix the toilet a lot. They have to fix the water recycling system a lot, and these are systems that need to be reliable for missions farther out, because you’re talking about a system working as well as possible to make sure the crew is going to be healthy and happy for a three-year mission to Mars.
To Mars, on Mars, the way back from Mars. Are these things that I guess from a human factor standpoint would be added stressors if we had to deal with maintaining systems and worrying about the reliability of these systems?
Dr. Brian Crucian:Well, you’re making excellent points, and I agree with what you’re saying, and you’re, I think what you’re basically saying is vehicle design for these missions beyond the Van Allen Belt is a very serious consideration.
Host:Oh, yeah.
Dr. Brian Crucian:And so we’ve got the ability to afford repairs on ISS if we have to. We can make a spacewalk. There’s enough room to have spare parts for a lot of different types of equipment. You’re simply not going to have those options in the far more dangerous environment of the lunar vicinity or transitioning to Mars.
[sound effect]
Host:And what that really comes down to is that systems have to be super reliable. Stan Love had some ideas on what that means for astronauts.
[sound effect]
Stan Love: The difficulty of transporting things to Mars means that we can take only the minimum amount of weight and things, and that includes spare parts. The space station right now was built, you know, of course we can send spare parts whenever we want, but the last four shuttle missions to space station carried nothing but gigantic, multi-ton palettes of spare parts that were affixed to the outside of space station, and those things are waiting. And we’ve used a few of those over the years since the shuttle program was cancelled, and, you know, we can’t afford to have a third of the mass of our Mars mission be spare parts. We’ll never be able to go. So that means we have to build machines that don’t break, ever. And we’re getting good at that in some areas. Jet engines, well there was a recent thing in the headlines with an engine through a turbine blade. The jet engines are incredibly reliable these days. You get millions of run hours, you know, before you get a failure. But if we could make everything on the spacecraft, especially that recycling equipment–
Host:Oh yeah.
Stan Love: That level of reliability, but now it has to be built with extra structural margin so that it doesn’t get cracks in it. You make things thicker. That makes them heavier. You have to test them for decades, right, that’s how long a jet engine can last, to make sure they’re going to last those years. So it becomes, you add weight, you add expense, you add development time to prove that things are that reliable.
[sound effect]
Dr. Brian Crucian:That’s a great point, and I think what you’re getting at is what if something goes wrong, either from a vehicle perspective or from a clinical perspective? And we actually have learned quite a bit on ISS about what happens if something goes wrong from a clinical perspective. In addition to researchers characterizing what is happening in astronauts, we also want to know if they become ill, and that is to a certain extent their confidential medical data. That’s not part of a research study, but for obvious reasons, we’re interested in what is the incidence of infectious disease onboard ISS. What happens onboard ISS clinically. And so we have an epidemiology group at the Johnson Space Center that very kindly compiled a lot of that data for us through the first 40 or so ISS expeditions in fact. They do have some degree of clinical incidence onboard station. We generally haven’t heard a lot about that. It’s not a tremendous amount. It’s nothing that’s of a serious concern, I think, for NASA or for the public, but it’s happening.
And so you have infectious diseases on board ISS. Some rare crews have some dermatitis issues that persist during flight, and so characterizing that on ISS is a very prudent thing to do because we don’t want things like that to get worse on the way to Mars. But you mentioned the return option, and yes, we have that rapid return option onboard ISS, and we won’t have that on the way to Mars. And so we very definitely need to characterize the human system onboard ISS during orbital space flight before we put it in this smaller, more constrained vehicle and put it out into this higher energy radiation environment for say a several-years mission to another planet.
Host:That’s right. Now based on what we know, from an immunology perspective, we talked a little bit with Dr. [inaudible] again, about medication. Do we know enough about immunology where, is there something universal that we can apply to the astronauts, maybe medication or maybe some sort of counter measure that can help prevent it, or is there a more personalized route that we really have to be considering, like a personalized medication or some kind of, I don’t know, something [inaudible]. I mean not sure.
Dr. Brian Crucian:Well, you made a very good point before when we were talking about getting a cold, and the medications you take after that or a treatment.
Host:Yeah.
Dr. Brian Crucian:And so you can look at the med kit onboard station and parse that out into okay what are the treatments, most of it is treatments, but what are the counter measures? And the counter measure is something that you’re going to take before you get sick.
Host:Right.
Dr. Brian Crucian:And try and prevent the development of illness because you’re fixing what’s broken in your physiology. And that is something that the community is still discussing, what will the counter measures be, what are the treatments. You also mentioned personalized medicine. And that’s going to be a very important part of biomedical counter measures for space flight. We have folks that are experts in this, Jeff Ginsberg in particular, who are starting to work with NASA and help us figure out how to take personalized medicine, precision medicine, and apply it to our unique problem, which is very healthy people in an adverse environment, and we want to keep them healthy. And so, we may need to be screening our astronauts at some point in the future. Do they have a predisposition to allergy or not? We might tailor a counter measure to them or for them based on their own personal history. If they get more infectious diseases than another crew member, we would like to know that. There are even some biomedical tests that you can perform to look at say their predisposition to inflammation or I’m speculating perhaps their individual microbiome, which latent viruses they are seropositive for and which ones they’re not.
The whole variety of things that we might consider looking at an individual astronauts as a screen prior to sending them on these exploration missions, because it would help us guide their personalized suite of counter measures.
Host:But it sounds like we sort, we already understand what we need to look for before we send someone out on a deep space mission. You’re already screening them, you’re already sort of understanding their physiology and what they may need to be successful on a space flight. Is that something that we can do, do a lot of testing beforehand and understand what we’ll need for a long trip?
Dr. Brian Crucian:Well, the answer is yes. We can do that. We’re not doing that yet. We don’t really have a need to do that for ISS missions. ISS is really the adverse environment that is near to us that we can use to characterize these phenomenon, and honestly we’re still learning. Even this many years into the lifespan of ISS, we’re still characterizing various biomedical phenomenon and learning. We recently learned that astronauts have a vision issue that were generally unaware of until a few years ago, and we’re learning about subtle aspects of the immune system response to space flight that we didn’t know until very recently. There are some very interesting articles that will be coming out soon. Dr. Rickey Simpson at the University of Arizona is going to publish an article looking at the function of natural killer cells, I mentioned those before, in astronauts. This was completely unknown before his study that in fact NK cell function is depressed in astronauts.
Host:Huh.
Dr. Brian Crucian:And that persists for a six-month mission. And so even now we’re still learning aspects of physiology that are altered that we may need to target these counter measures for.
Host:Wow. So is there something that we can do I guess before space flight. Like what are we doing before they even launch to really make sure that they are going to be successful, at least right now for the space station. Is there counter measures or preparation studies that we’re doing to understand this information?
Dr. Brian Crucian:So we are not really implementing specific immune countermeasures. And in fact, our biomedical elements within the human research program are all collectively working to characterize their systems and talk about their counter measures. You have had some successful counter measures. Potassium citrate, Dr. Peggy Wittson was the principal investigator for a study that looked at renal stone risk onboard ISS and successfully validated using potassium citrate pills as a counter measure for that. But generally, we’re all a little less mature in our counter measures development. And so collectively, the disciplines within the human research program are looking at this. You’re going to see more translational counter measures be discussed. I’ve heard of the integrated counter measures suite, and so it’s impossible to implement a counter measure for one system and not have it influence another system. Your immune counter measures are probably going to have a positive or negative influence on bone, cardio, [inaudible] pathogen interactions, and conversely, just about any counter measure you can think someone might implement for another system, say exercise, is going to positive affect immune.
And so really you have a lot of integration in NASA’s approach to looking at the problems and in the develop of the counter measures.
Host:So looking kind of forward to let’s just say we have a long duration stay on the moon. We’re looking at the moon to really get more data to understand what’s needed to go even further out, to have a habitat on Mars. What are some of the interesting things if we were to have a long duration mission, say six months, maybe even a year on the moon, that can really give us insight into even missions even farther out, from an immune perspective.
Dr. Brian Crucian:Well, the moon is a very interesting place.
Host:Yeah.
Dr. Brian Crucian:And from an immune perspective, we really feel that the destination almost doesn’t matter. When you’re beyond the Van Allen Belt and you increase the radiation and you increase the stress and you’re living in constant microgravity, it doesn’t matter where you go. You’re probably going to manifest the same types of immune problems from one destination to another. Living on the moon is an interesting consideration though because you’re not in pure microgravity. Now you’re in one-sixth gravity.
Host:Right.
Dr. Brian Crucian:And so I don’t think anybody knows, if you look at a moving scale from zero gravity to one times the force of gravity we have here, where does the problem start. Is half gravity enough? Is one-sixth enough? I don’t think anybody knows. There have been some fractional gravity bedrest studies that have been implemented, but I don’t think they really were able to look at the immune system because bedrest isn’t the best analog, I don’t believe, for the immune system. But it is something that folks are aware of. There has been an artificial gravity study that NASA worked at in Galveston at the University of UTMB down there, UTMB, in Galveston, sorry. You can stitch that together, that looked at artificial gravity as a countermeasure, and so, yeah, fractional, when you talk about the moon, you’re really talking about fractional gravitational forces and what’s the effect of that on physiology, and that’s an area I don’t think anybody has really been able to investigate.
It’s very difficult to investigate that on Earth, because you’re in a constant 1G field, and you just can’t get away from it as much as it would be great to have that 0G room, we just don’t have that.
Host:So it seems like gravity is just a consideration for a lot of different things, talking with a lot of the other experts, it’s for this immune system. It’s for the crew behavioral health. Fluid shifts. You know, there’s a lot of exercise, bone, muscle loss, a lot of things that are associated with just this lack of understanding of what happens in the one-sixth gravity environment.
Dr. Brian Crucian:Yeah. We evolved as people in a constant 1G field, and no one had ever been out of it until the first astronauts and cosmonauts launched in the ’60’s, and I don’t think anybody fully realized what being outside of gravity can do to your body. And we see astronauts working very successfully and enjoying their stays onboard ISS, but if you take cells out of the body, immune cells out of the body, I can pull T cells from your blood right now, and if we put them in culture and we stimulate them and try and re-create an immune response, they literally don’t work. They don’t respond.
Host:Huh.
Dr. Brian Crucian:And that is absent stress, radiation, or anything else. Just having these cells cultured in microgravity, they don’t respond. And so investigators on the ground, NASA and external investigators have been doing flight studies of cell culture and culturing cells in ground-based apparatuses, ground-based apparatus, such as a bioreactor, which mimics microgravity culture to try and figure out why, and it appears that there are gravity-sensitive weight points in say the signal transduction pathways where the cell tells the nucleus how to respond, that are gravity sensitive. Who would have ever thought that our cells would have a gravity-sensitive weight point within them and that they would stop working in microgravity, and yet that appears to be the case.
Host:Wow. I don’t even know what you do with that. I mean there’s not like, there’s no like pill you can take. I mean like there’s a gravity pill– yeah, that’s a huge consideration.
Dr. Brian Crucian:Well, there’s a couple things you could do. I mean there are immune boosters, immune stimuli that might help overcome this effect to some degree. People have considered artificial gravity as a counter measure. Seen 2001 of Space Odyssey, if you could rotate the vehicle and get gravity back, it might help mitigate some of those effects. But also, I mentioned that we can pull cells out of you and me, stimulate them to microgravity and they wouldn’t respond. And yet, the astronauts are very healthy on orbit. So we don’t necessarily know if that phenomenon is reproduced inside the body, because the cells in the body are not just floating in a pristine microgravity environment. They’re moving. They’re moving through the blood, and they’re migrating in and out of tissues and they’re looking for targets to respond to to keep you healthy. So it’s a, where we’re bringing this home to is it’s a very complicated consideration. Every system is complicated.
In particular, the immune system, all these cells and the environment they have to function in and keeping them functioning properly to maintain our health, it’s a complicated consideration.
Host:I think that’s actually a good place to start wrapping up because this is the end of our hazards series. This is the last episode, and the theme that I’ve sort of heard throughout this entire series so far is we’ve sectioned off each of the hazards and really gone deep into what those hazards mean, but throughout my talks the all of the experts, all of you guys, what I’ve really learned is that everything is connected. You can’t just look at just the immune system. You got to think about what the gravity is doing and what the bone and muscle is doing and what, you know, how does fluid shifts go into this, going far away. You know, everything is, everything is connected. So, you know, one thing we talked about actually with another, Dr. Eric Antonsen, you know, we just talked to them, so it’s all fresh in my mind, that particular talk, but we were talking about how all the experts are getting together and providing input. So when you are getting together and talking about this deep space exploration, what are some of the key things that you try to, that you try to make sure that we are implementing into our future space flight plans?
Dr. Brian Crucian:So you’re absolutely right, and we actually have a name for that phenomenon and what you’re describing is interdisciplinary science or translational science. And we have collectively learned that as a team over the lifespan of ISS, as the nutrition folks have, Dr. Scott Smith’s lab at JSC have looked at inflammation and bone markers and nutritional status, and they have been talking to the immune team down the hall, and we’ve been looking at immune mediators, and we’re starting to connect the dots between these systems. We’ve learned what exercise can do to the immune system, what fluid shifts can do to the immune system, and what inflammation does to a variety of systems. And so we have a name for that phenomenon, and as you so aptly put, we’re working together now collectively, more than we ever have before, to address clinical risk to crew members as sort of a unified team of investigators across all of these disciplines. You asked what we’ll do about this going forward, and so you’re seeing more joint solicitations for science projects or translational solicitations.
Instead of NASA or an agency looking to do a cardio study or an immune study, you’re seeing broader solicitations now where the agencies that fund are encouraging investigators to look at translational aspects of their system or their findings and also interdisciplinary interpretations of data. An immune study that was completed years ago, we now have folks pulling some of that information. Dr. Han Lu Wu in NASA radiation is pulling some of the immune data from a study several years ago where he had radiation data. So he’s looking at say inflammation and correlating that with radiation to see if there’s a relationship there. And so the bottom line is more translational work, more interdisciplinary work, looking at these things together within our areas in JSC and also with European scientists, Canadian, Japan, Russian. We have several very interesting studies that the Japanese Space Agency is working on, looking at [inaudible] analyses of astronauts on the International Space Station or probiotics as a counter measure.
We’re very excited to see these studies mature and the data that they’ll show, and it just keeps feeding more information that all of us use to help to close our clinical risks to crew members for these pending exploration missions.
Host:Collaboration is so important, but I did want to end on a more selfish note. And that is, what are you, from your immunology perspective, looking forward to most for these deep space missions, to figure out?
Dr. Brian Crucian:Well, I’ll answer first selfishly. I’m looking forward to just seeing them happen. I’m 50 now, and so I’m very excited to see people go beyond the Van Allen Belt and get to doing some real space exploration. As a scientist, I’m looking forward to basically characterizing our system, the immune system as much as possible and start to have that dialogue about counter measures. As I alluded to before, we’ve got a big suite of counter measure options for immunology. Nutritional supplements, functional foods, probiotics, medications. And so we plan to have discussions here within the next couple of years where we will engage flight surgeons, researchers, practicing clinical immunologists, people that are actually treating patients. We want them to come here, see our data, and help us figure out what would be the best counter measure for astronauts on a three-year mission to Mars. After we make that decision, then we’ll have to probably spend some time looking at these counter measures, validating them in a ground analog, or hopefully onboard ISS, on ISS before the end of its lifespan so that we can have these counter measures ready for these deep space exploration missions.
Host:I’m very excited for it. Brian, thank you so much for coming on and sharing your perspective about these hostile and closed environments, especially from the immunology perspective. I really appreciate.
Dr. Brian Crucian:I’ve enjoyed it. Thank you for having me.
[ Music ]
Host:Hey, thanks for sticking around. So today we talked with Dr. Brian Crucian about immunology and that aspect of the hostile and closed environments. That wraps up our five hazards of human space flight podcast episodes. You can go back and listen to previous episodes. They’re not in really any particular order, but we have associated products that go with those. If you go to NASA.gov/hrp, there’s a series of videos that are associated with each of these five hazards that are short animation videos, really give you a nice kind of overview perspective. You can go there to watch those videos. Otherwise, a lot of the stuff that we talked about today and a lot of our podcasts happen on the International Space Station, go to NASA.gov/ISS to find the latest there. On social media, that’s where we’re looking for our questions and really answering them here on today’s podcast. On Facebook, Twitter and Instagram, you can use the #askNASA on the International Space Station or NASA Johnson Space Center accounts to ask a question or maybe submit an idea for an episode that you’d really like us to dive deep into, for Houston We Have a Podcast. Just make sure to mention Houston We Have a Podcast. That’s how I find it. Because there’s a lot of ask NASA questions that we actually cover.
So this episode was recorded on June 28, 2018. Thanks to Alex Perryman, Pat Ryan, Bill Stafford, Bill Polaski, Judy Hayes, Isidro Reyna, Mel Whiting, and Natalie Gogins. And thanks again to Brian Crucian for coming on the show. To our listeners, thanks for joining us for this special series on the hazards of human space flight. We’ll be back next week with your regularly scheduled programming.