At the age of 11, Theresa Beech’s son Daniel was diagnosed with osteosarcoma, the most common bone cancer according to the American Cancer Society. It is considered by many among the toughest to treat. While Daniel was on hospice, Theresa, unsatisfied with the status quo, identified drugs not typically used in osteosarcoma treatment and convinced doctors to prescribe them.
“Doctors believe these drugs may have extended Daniel’s life by up to six precious months,” said Theresa.
While Daniel was on hospice, Theresa began investigating the genetics of osteosarcoma tumors, applying her engineering skills to cell biology. With the help of other parents of osteosarcoma patients, she compiled the Patient/parent Osteosarcoma genome-Wide Registry, or POWR, which is believed to be largest osteosarcoma genomic and medical history data set ever assembled.
Analyzing this data set as she would a space communications network for vulnerabilities, Theresa identified a gene that, when targeted with medication, might provide better outcomes for those suffering from her son’s disease.
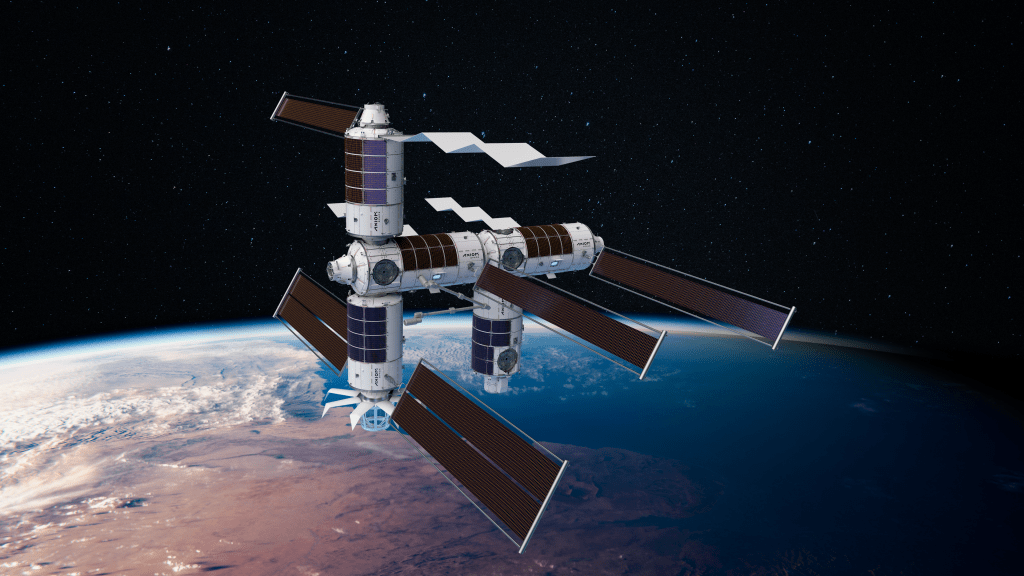
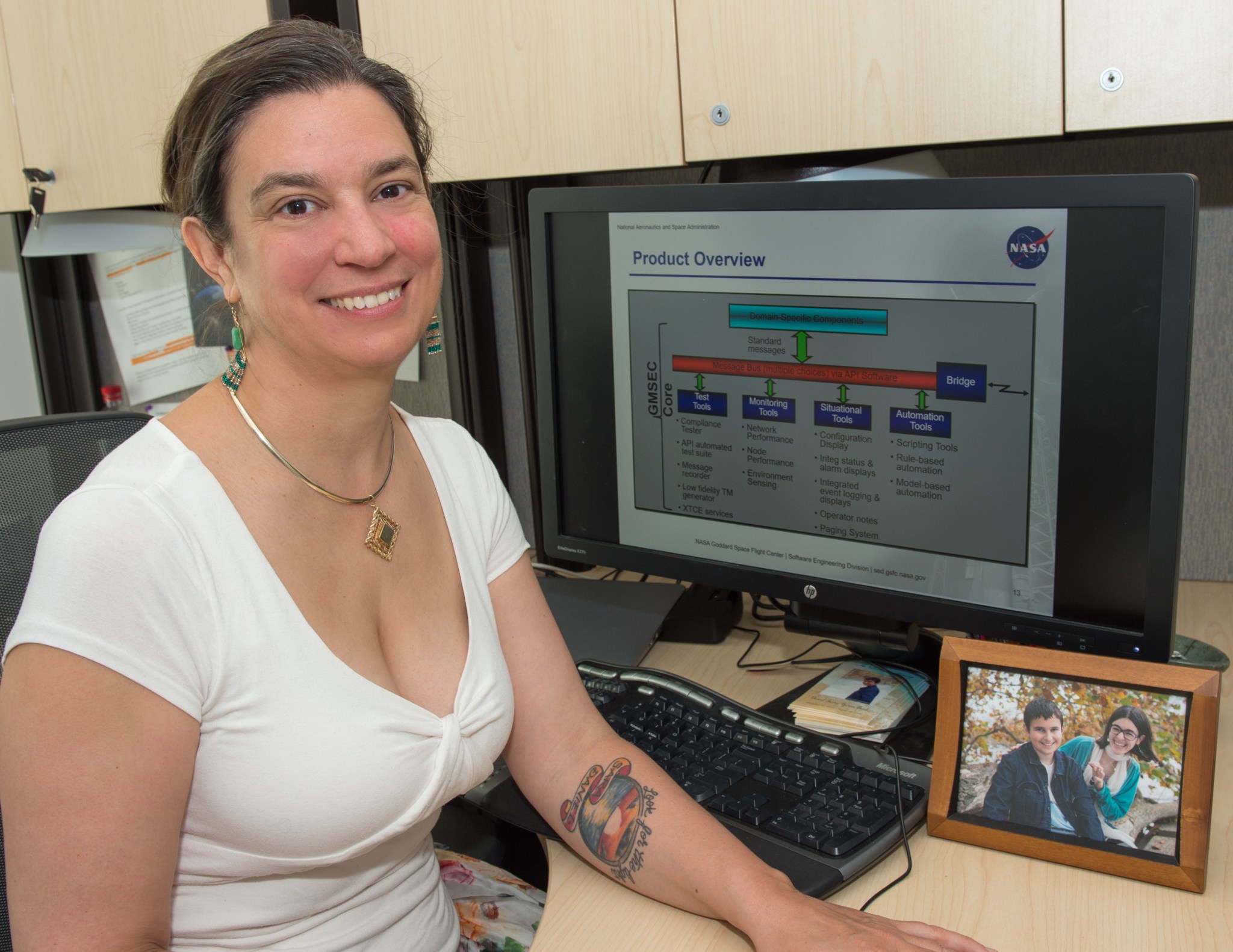
Theresa has worked in space communications’ commercial sector for over 15 years. She recently came to NASA’s Goddard Space Flight Center, lending her expertise to the agency as product development lead for the Goddard Mission Services Evolution Center (GMSEC).
What specifically is the nature of your work in GMSEC?
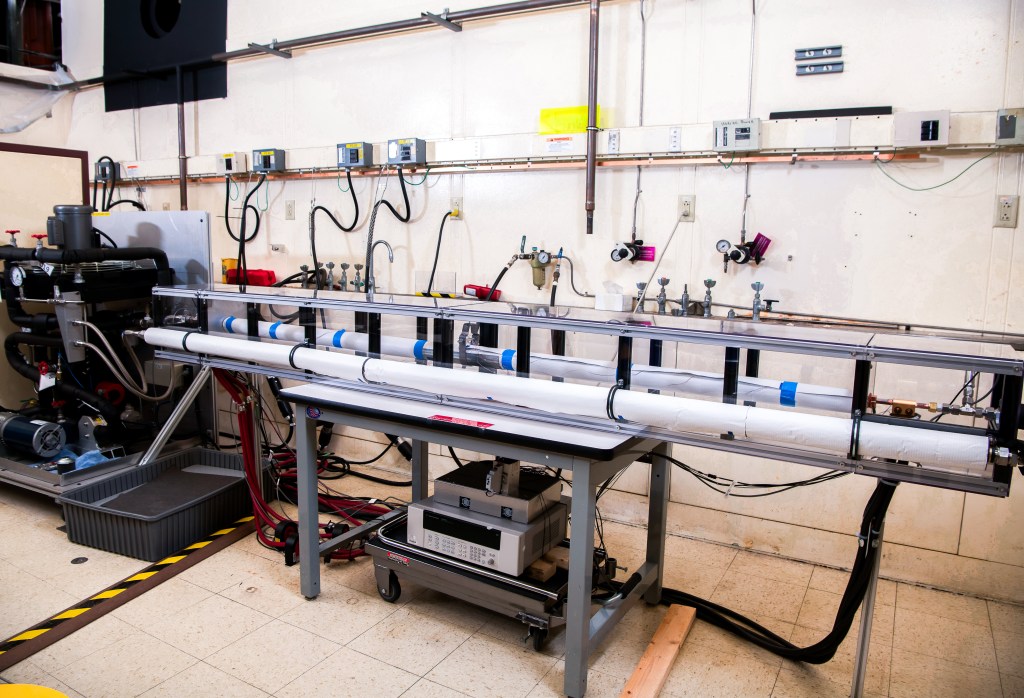
My official title is “product development lead for GMSEC.” Essentially, I lead the technical team. There’s about 12 to 15 engineers working on GMSEC. We provide ground systems support to customers across NASA and the U.S. government.
Space is an artisanal world. Every satellite is unique. You occasionally get spacecraft that are built to spec, but usually each mission has unique requirements for their ground network. Acknowledging this, GMSEC take this highly custom field and defines a common architecture, developing software that addresses it and building customized architectures from there.
What are the advantages to using GMSEC software?
Using GMSEC gives missions a more robust ground system. We provide tools for things like anomaly and situational management. Some of the larger missions will spend time building this robustness into their ground systems, but we offer smaller missions a similarly resilient communications architecture.
It also becomes very expensive to replace parts if you’ve done a custom ground system. Using GMSEC’s approach, the majority of your interfaces are standard, so changing out components and software systems becomes significantly easier and cheaper.
From a training perspective, operators moving between missions can spend less time learning a new console. They have a series of common tools they can rely on across many missions.
You’ve said that a communications network looks and performs like a cancer cell. How did your knowledge as a systems engineer enable your cancer research?
You have to understand that this was a crazy idea I came up with at one in the morning, grieving Daniel’s death and deeply sleep deprived.
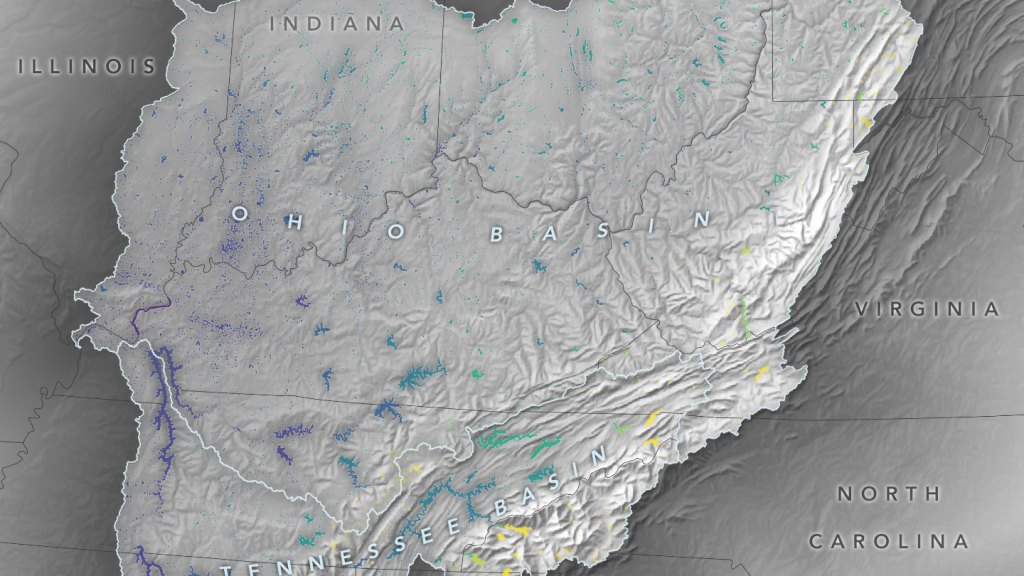
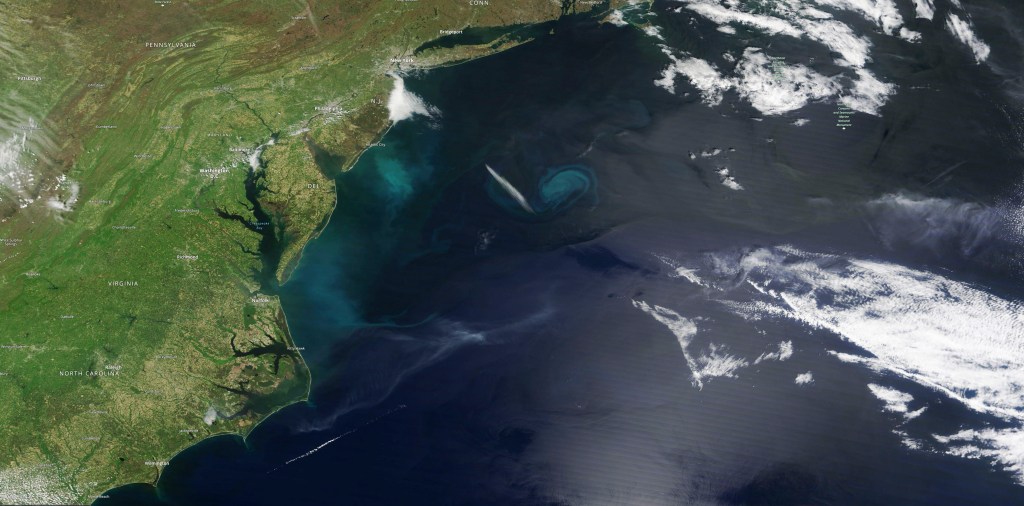
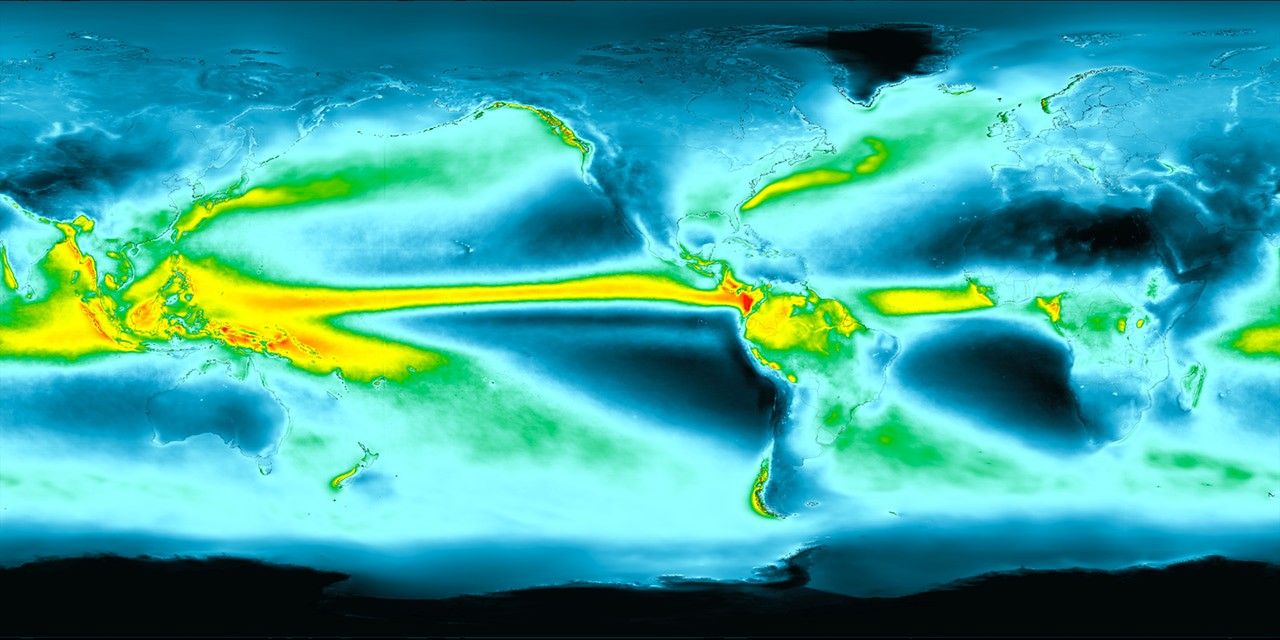
Basically, when looking at a communications network for vulnerabilities you identify choke points, areas of high traffic. If one of these nodes goes down, you could have a major interruption in service, so you build redundancy around it. A network could have many of these choke points depending on its complexity.
Traditionally, cancer researchers talk about cell signaling pathways. I thought, “Well, it doesn’t really behave like a pathway. What if it’s not a pathway? What if it’s a network? If it’s a network, can I identify a choke point and exploit that vulnerability?”
Researching cell genomics, I looked for a biological proxy for communications traffic. I found micro-RNA, which basically pass genetic signals through the cell. There’s been research into which micro-RNA are involved in osteosarcoma, so I traced them to the genes they impact.
What was the result of this research? Could you identify a choke point?
One gene kept showing up: ROCK1. I found a paper from about 10 years back that had checked a number of osteosarcoma tumors for ROCK1 expression — they had found that ROCK1 expression correlated highly with death in patients. Then I found a drug that targets ROCK1 to treat heart attacks and strokes that’s been around for 20-some years.
Dr. Rosie Kaplan, a pediatric oncologist and researcher at the National Cancer Institute, thought the drug might work in treatment because it impacts the tumor micro-environment. She’s found that the drug can actually kill osteosarcoma cells in the lab.
A clinical trial would help to see whether this could become a viable treatment option.
I’d love to ask you about the nature of service: of your service to Daniel and to all those suffering from osteosarcoma. What inspired you to delve this deep?
I grew up in a family that believed actions count more than words. We all say pretty words. We all say we love our kids, that they’re the most important thing. But it’s our actions that matter.
Some parents can raise funds for research; I’m useless at raising money. Some parents can lobby the government; I don’t have those connections.
I’m an engineer — I use what I have.
I love my son. I will always love him. I would have done anything to save his life, but I couldn’t. He died — lots of kids die — because this disease is difficult to treat. Our kids deserve better.
If, by using my engineering abilities, I can help kids, then I feel I have do that. As Emily Dickinson wrote, “If I can save one heart from breaking, I shall not live in vain.”
To learn more about Theresa’s work with GMSEC, visit their website. Outside of NASA, Theresa continues her osteosarcoma research and advocacy through a non-profit organization she founded that raises funds for and awareness of osteosarcoma clinical trials.
By Danny Baird
NASA’s Goddard Space Flight Center